Is your central line procedure decreasing patient safety?
Learn how to use the human factors in healthcare to help prevent CLABSI.
In most cases, people choose to become clinicians out of a deep commitment to patient care. But like everyone else, clinicians are human beings. They can become tired, overworked and overwhelmed by the everyday demands of caring for multiple patients—and even more so when caring for more and sicker patients during a pandemic. Lapses in practice can happen in a busy healthcare facility with limited staff, impacting patient care and safety.
This isn’t just a theory. In healthcare settings, human failure can cause up to 90% of such errors,1 including the kind that can lead to central line-associated bloodstream infections (CLABSIs). Medline’s BSI 2019 Discovery Assessment Findings reported that more than half of observed clinicians didn’t maintain aseptic technique every time they changed a catheter dressing. And 60% didn’t always prepare a clean area for the dressing change kit.2
How do you improve performance at your facility? By using human factors analysis, or human factors engineering.1
Human factors is a human-centered science using tools and methods to enhance the understanding around human behavior, cognition, and physical capabilities and limitations. You can then apply this knowledge to design systems that support these capabilities and limitations. This approach can lead to practical changes across your system, making it easier for frontline staff to keep patients safe.1
60%
of observed clinicians didn’t always prepare a clean area for a dressing change kit2
How can human factors analysis help improve patient care and safety? Here are three strategies—designed with human factors in mind—to help your team prevent CLABSIs.
1
Standardize product supply and procedure steps
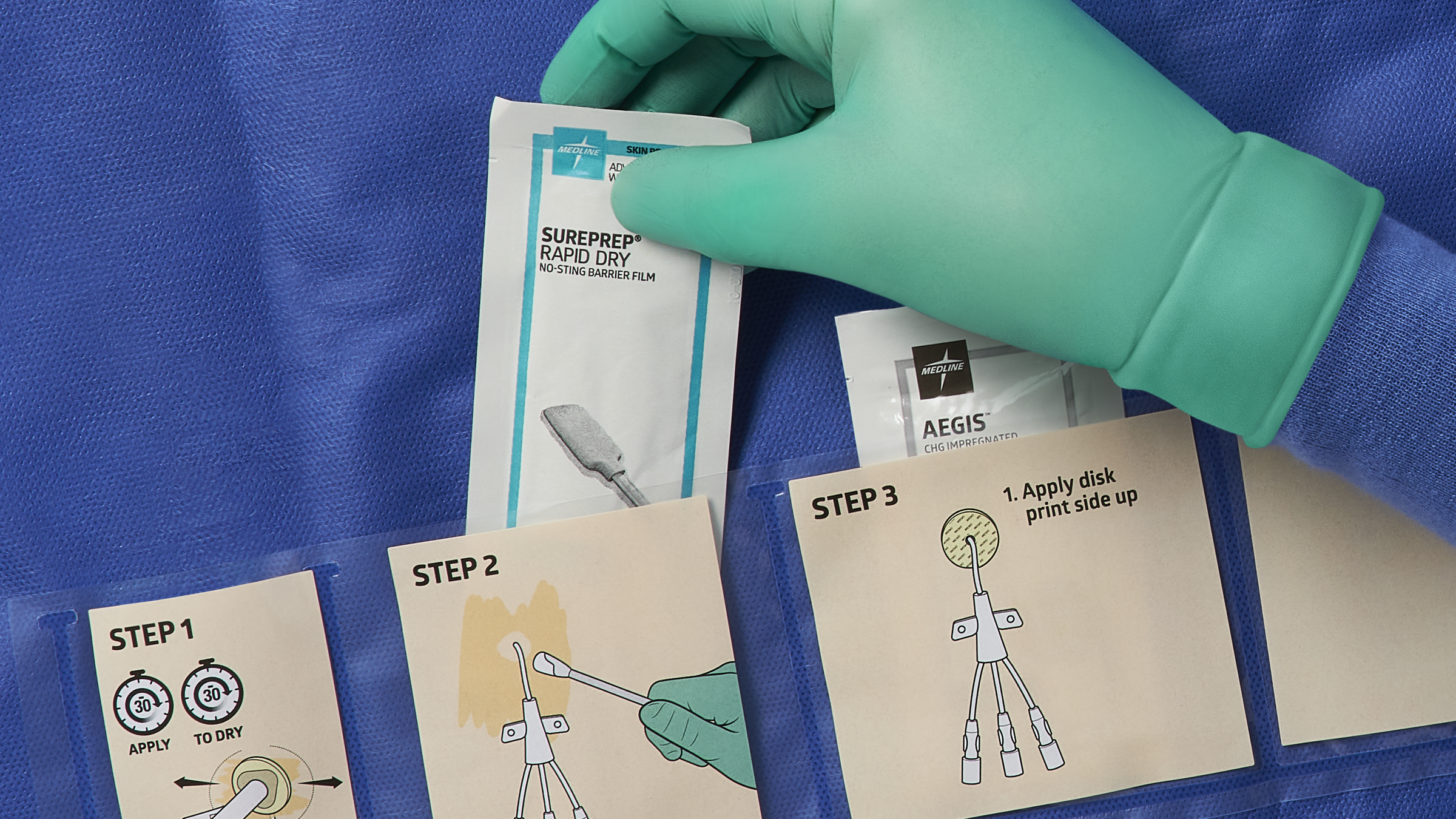
Not having readily available supplies or having too many supplies on hand can lead to errors. When clinicians have to pull each item separately for a procedure, it can be all too easy for them to miss components or steps. When they have too many product options to choose from, it can cause confusion about what to use. Both situations “create opportunities for variability, which can impact errors,” says Donna Matocha, Medline Manager of Clinical Resources – Critical Care.
“The human factors-based solution is to use all-encompassing bundles for CVC insertion and maintenance,” explains Matocha. “These can help you make sure that every clinician can easily perform a consistent procedure using standardized products.”
Including a simple checklist that summarizes every step that clinicians should follow can also help reduce variation. This practice is especially useful in settings where travel nurses frequently work.
2
Empower your team with education and training
Too often, clinicians don’t have the time or opportunity to receive training. And if they do get training, it’s usually for only a few minutes during rounds. That’s a problem, says Vincent Tessitore, Medline Clinical Resource Manager – Critical Care.
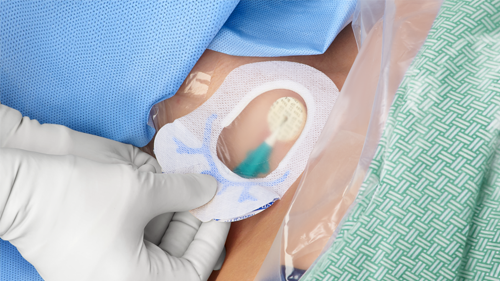
Consider this: Medline’s findings revealed that a quarter of observed clinicians didn’t use a securement device when inserting a catheter.2 And 29% didn’t properly apply a chlorhexidine gluconate (CHG) dressing to disinfect the insertion site.2 In-person training and practical demonstrations of dressing change and line access protocols can help drive compliance in these areas.
“But putting clinicians in the position of having to learn from a quick presentation at the nurses’ station when they have conflicting priorities isn’t effective,” says Tessitore.
29%
of observed clinicians didn’t properly apply a CHG dressing to disinfect the insertion site2
He recommends 30-minute training sessions that take place away from the bedside. Education materials such as posters and easily accessible online courses and learning modules can also support education goals. But clinicians need to be able to review them on a schedule that’s easy for them to balance with patient care. That way “the patient is getting the best benefits,” says Tessitore.
3
Create a collaborative, team-based culture
Inconsistency in prevention practices across units can be a major reason for higher CLABSI rates. For instance, Medline’s analysis showed that in observed dressing changes, 44% of nurses didn’t perform hand hygiene appropriately.2
A unit-based champion strategy can help you reduce practice variation across all units. Clinicians with strong knowledge of prevention guidelines can serve as leaders in their units, helping motivate their colleagues with demonstrations and visual aids. For example, they can post hand hygiene reminder signs in patient rooms within their unit.
Evidence shows that it works. Through the On the CUSP: Stop BSI project, unit champions in different hospitals were designated to empower colleagues to follow CLABSI prevention best practices. States that participated in the project reduced CLABSI rates in their ICUs by 41%.6
“When you can get clinicians engaged, you’re creating shared responsibility for reducing infections,” says Tessitore.
Key takeaway
You can be more successful at reducing CLABSIs and other healthcare-associated infections (HAIs) by incorporating human factors-based solutions in your prevention plan. Human factors analysis focuses on identifying ways to prevent human error. Too many supplies, inconsistent training, and differing levels of clinical expertise and experience can lead to practice variation. Addressing these issues head-on with intuitively designed products, comprehensive education and a collaborative strategy can help you drive a culture of safety across your organization.
References:
- Human factors analysis in patient safety systems. (2015, April). The Joint Commission. The Source. 13(4). https://www.jointcommission.org/-/media/deprecated-unorganized/imported-assets/tjc/system-folders/assetmanager/humanfactorsthe_sourcepdf.pdf
- BSI 2019 discovery assessment findings. Medline Industries, LP. https://meddevod.wpdev.medline.com/media/catalog/Docs/MKT/WP/OTH-EBSI-Discovery-Assessment-Overview-11-20.pdf
- Association for Professionals in Infection Control and Epidemiology. Guide to preventing central line-associated bloodstream infections. APIC Implementation Guides. (2015, December). http://apic.org/Professional-Practice/Implementation-guides/#implementaion-guide-7464
- Guidelines for the prevention of intravascular catheter-related infections. (2011). O’Grady, NP; Alexander M; Burns, LA; et al. Centers for Disease Control and Prevention website. https://www.cdc.gov/infectioncontrol/pdf/guidelines/bsi-guidelines-H.pdf
- Marschall, J; Mermel, LA; Fakih, M; et al. Strategies to prevent central line-associated bloodstream infections in acute care hospitals: 2014 Update. Infection Control and Hospital Epidemiology, Vol. 35, No. 7 (July 2014), pp. 753-771. https://www.jstor.org/stable/10.1086/676533.
- Eliminating CLABSI, A National Patient Safety Imperative Final Report on the National On the CUSP: Stop BSI Project. (2012, October). AHRQ. https://www.ahrq.gov/sites/default/files/publications/files/clabsifinal.pdf