Hand hygiene in healthcare: The 6 essential elements
These best practices can help reduce infection rates across your facility.
Everyone who enters a healthcare facility has the right to expect the highest standards for patient/resident safety and quality. One of the most fundamental ways to achieve these standards is to create and value a culture in which hand hygiene is second nature.
Given that compliance rates—when measured accurately and reliably—typically fall below 50%, a sound and evidence-based strategic framework is essential to drive sustained improvement. Such an approach provides a checklist of hand hygiene program elements that all work together to ensure optimized hand hygiene behavior.
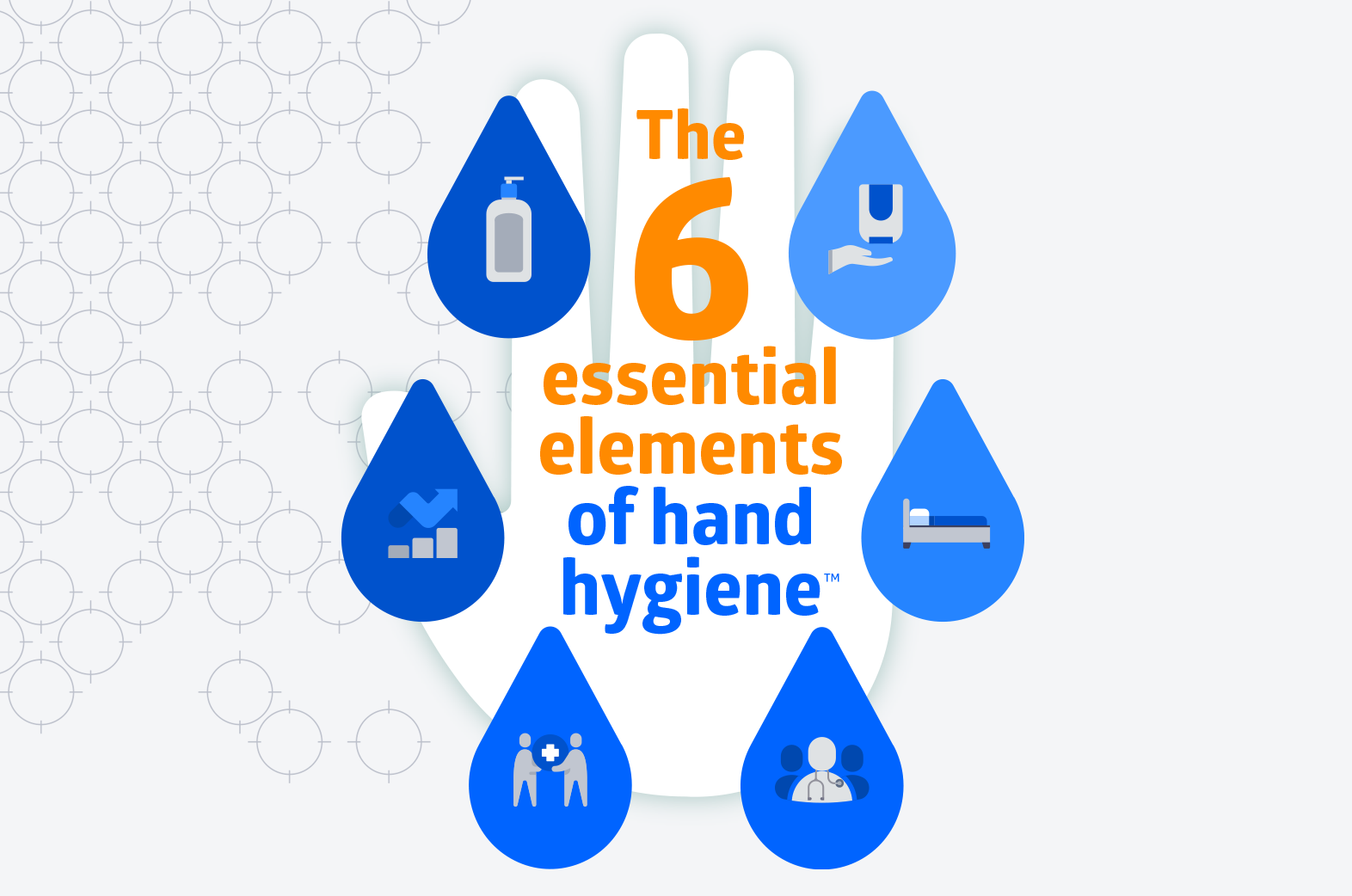
About a year ago, we introduced a strategic framework, “The 6 Essential Elements of Hand Hygiene™,” to help make hand hygiene second nature for all. Over the past year, we’ve refined our framework to make it easier to implement across your facility. Feel free to share this educational tool with your infection prevention, epidemiology, patient/resident safety and quality leadership teams.
6 essential elements of hand hygiene
1 | Advanced products
Select a standardized product formulary that is supported by sound science and developed for high frequency hand hygiene. Ensure that staff acceptance is widespread before implementing:
- Alcohol-based hand sanitizers
- Soaps (plain and/or antibacterial)
- Alcohol-based sanitizing wipes
2 | Reliable delivery systems
Align placement of product dispensers with CMS, CDC, Joint Commission and WHO guidelines such as:
- Wall-mounted hand sanitizer dispensers (manual and/or touch-free) inside and outside of patient/resident rooms
- Soap dispensers at all sinks
- Consider lotion dispensers adjacent to sinks to best maintain skin health (lotions should be latex/nitrile plus CHG compatible)
- Touch-free hand sanitizer dispensers on stands for entryways and other open areas—place easy-to-read signs on top to encourage use
- Personal carry-size hand sanitizer bottles
- Tabletop pump bottles with soap and/or sanitizer as appropriate where access to wall-mounted dispensers is limited
- Alcohol-based sanitizing wipes in packets and canisters
3 | Point of care access
Position hand hygiene products close to where hand hygiene moments occur:
- Outside and inside patient/resident rooms
- At the bedside
- Throughout the OR (for acute care facilities and ASCs)
- At nurse stations
- In treatment and examination rooms
- In food service, dining and food preparation areas
- At information, reception and gift shop desks and counters
- In entryways and lobbies
Provide personal carry-size bottles for when access to wall-mounted dispensers is limited or inconvenient
4 | Effective learning systems
Provide targeted education and training tools (based on behavioral science, human factors and high-reliability organizational design) to make hand hygiene best practices second nature for all:
- Organizational leadership
- Staff and volunteers
- Patients/residents, families and visitors
Ensure tools emphasize proper technique at every moment:
- Before and after touching the patient/resident and/or their surroundings
- Before and after patient/resident care tasks (changing dressings, inserting new lines, etc.)
- Before and after personal activities such as eating, handling a cell phone or device and using the restroom
Deploy facility-wide reminders (rotate them regularly to keep the motivation fresh):
- Posters
- Elevator wraps
- Tent cards in dining areas
- Patient/resident and family informational brochures
- In-house TV hand hygiene reminders (think public service announcements or PSAs)
- Notices on facility’s website and/or apps
5 | Safety culture
Foster a safety culture that embraces:
- Leadership engagement and modeling of expected hand hygiene behaviors at all times
- Psychological safety—everyone feels safe to speak up when a hand hygiene opportunity is missed and greets such reminders with a “thank you!”
- A top-down accountability framework with a unit-based approach for barrier removal, action planning, goal setting and celebrating of gains
6 | Actionable feedback
Implement best practices for collecting and analyzing data, and understand how to pinpoint where improvement is needed:
- Implement reliable performance measurement methods (e.g., electronic hand hygiene compliance monitoring)
- Provide timely, actionable feedback to all
- Maintain and distribute individual hand hygiene report cards to frontline staff so they can be aware of and improve personal practice
We’re excited to bring you this framework and think it will go a long way in helping your leadership think about hand hygiene in a systematic way that contributes to high staff performance with sustained compliance improvement.
As you think about organizational goals for 2022, consider incorporating the framework as a new patient/resident safety and healthcare quality tool.

VP Patient Safety Innovation for Medline Industries, LP
Paul invented the first electronic hand hygiene monitoring system designed to improve hand hygiene performance while reducing infections and costs. He is an innovative and mission-driven leader with more than 35 years of experience in hand hygiene and patient safety solutions. Paul also shared hand hygiene insights as a past contributor to Healthcare Hygiene Magazine.
Disclosure: Medline is a 2021 member of the Leapfrog Partners Advisory Committee and has a collaborative relationship with a company that offers electronic hand hygiene monitoring services.




