Nurses reveal pressure injury prevention education they need
Survey confirms, it’s time to refocus on the basics of prevention.
Pressure injuries can be painful and often negatively impact a person’s quality of life. They’re also notoriously expensive to treat, due to costs of products, labor and potential associated fines.
That’s why you do everything you can to prevent pressure injuries before they happen. But the pandemic forced many of you to shift your attention away from pressure injury prevention.
As COVID-19 cases continue to fluxtuate, you’ll know when you’re ready to think about how to refocus on the basics of PI prevention. To help you do that, Medline conducted a survey of more than 250 clinicians (wound care nurses, registered nurses and others),¹ asking what nurses like you have been doing and feeling about prevention protocols and education since March 2020.
Here, we discuss some of the key learnings based on the survey feedback and how you can incorporate them into your daily practice.
COVID-19 affected PI prevention
As the number of critically ill patients and residents increased, caregivers suddenly needed to redirect their time and resources away from skin health. On top of that, you experienced staffing shortages, PPE shortages, burned-out nurses and social-distancing requirements.
The consequence: Prevention efforts and prevention education both waned.
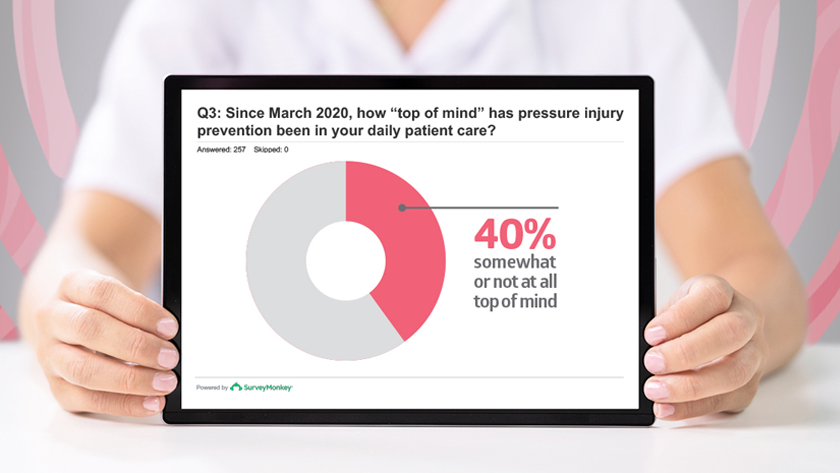
According to the survey, 40% of respondents felt that pressure injury prevention was only somewhat or not at all top of mind at their facility.
One survey respondent put it bluntly: “There has been much less focus on pressure injury prevention during COVID outbreaks. Saving lives takes priority over skin health.”
40%
of nurses said PI prevention was somewhat or not at all top of mind¹
Shifting priorities back to prevention
According to the survey, one important aspect of pressure injury prevention that slipped during the pandemic was the routine meeting of skin champion teams and other skin care quality initiatives. Nearly 30% of surveyed nurses said these meetings to support skin health were put on hold.
Skin champions and quality initiative members often serve as anchors for pressure injury prevention; losing those anchors also means losing a powerful avenue for sharing learnings and reinforcing evidence-based best practices across all areas.
“Saving lives takes priority over skin health.”
Read on to learn more about what the survey revealed and how the findings can inspire your team to refocus on the basics of prevention. We look at this as a full prevention toolkit including evidence-best practice guidance, valuable education and the right system of products.
Promote evidence-based best practices focused on prevention
Nursing staff may be aware of evidence-based best practices, but survey responses indicate there have been gaps in practice since March 2020.
86%
of nurses said they should be doing more repositioning and offloading
62%
of nurses said they should be doing more to focus on everyday skin care
47%
of nurses said they should be doing more to improve nutrition
When nurses were asked what they felt they should be doing more of to help prevent pressure injuries, these three answers stood out:
- Repositioning and offloading: 86% of nurses said they should be doing more to help reposition and offload fragile skin. Staff has been pulled in other directions to care for patients and residents with COVID-19, which may have resulted in inconsistent repositioning and offloading practices. As COVID-19 treatment becomes more systematic, nurses recognize the importance of improving their repositioning protocols. A smart place to start is by encouraging staff to follow National Pressure Injury Advisory Panel (NPIAP) guidelines. NPIAP best practices call for frequent pressure redistribution, along with regular skin assessments to help identify early stages of pressure injury formation.²
- Daily skin care: It takes time to cleanse, moisturize and protect each person’s skin properly, and the majority of nurses surveyed recognize the benefits. In fact, 62% of those surveyed said they feel they should be doing more to focus on everyday skin care. When it comes to reducing the likelihood of pressure injuries, optimal skin health is key. An added bonus to conducting regular skin care is that it provides a great time to reassess people’s skin for any early signs of injury.
- Nutrition: 47% of nurses said they should be doing more to improve nutrition for their patients and residents. In fact, that number seems low considering that the NPIAP states, “Both inadequate nutritional intake and undernutrition have been linked to the development of pressure injuries, pressure injury severity and protracted healing.”² The NPIAP guideline presents several recommendations regarding nutrition and pressure injury prevention, including the importance of considering the “impact of impaired nutritional status on the risk of pressure injuries” and conducting nutritional screenings for at-risk individuals.² Consult with a dietitian to determine whether a supplement makes sense.
Dispel 4 myths of pressure injury prevention
As you begin to refocus on the basics of prevention, be sure not to fall into any “old ways” of thinking.
Myth 1: Applying a sacral dressing means your job is done
National Pressure Injury Advisory Panel (NPIAP) clinical guidelines recommend at-risk individuals receive a soft silicone multi-layered foam dressing, not on its own, but rather in conjunction with other prevention measures.² Studies show that including this practice as part of a skin care bundle can reduce pressure injury incidence.
Myth 2: Turning patients every two hours is best
Every two hours is an outdated turning and repositioning protocol. According to the updated NPIAP 2019 guidelines, the frequency should be determined on an individual basis, depending on a person’s activity levels and their ability to reposition themselves.² Besides starting with the right support surface, consider the following characteristics of each individual:
- Skin and tissue tolerance
- General medical condition
- Overall treatment objectives
- Comfort and pain
Myth 3: A little is good, a lot is better
Sounds logical, but that’s not usually the case. It’s important to follow the product application instructions, because sometimes over-applying a product can cause damage. For instance, barrier products can crack if too much is used, which breaks the seal and allows moisture in, instead of keeping it out.² It’s also inefficient and can unnecessarily drive up your cost of skin care.
Myth 4: The job of the CNA is to perform the mundane tasks
Certified nursing assistants interact with patients and residents typically more than any other caregiver. They get to know the people they care for, and a lot of that care is personal. “Oftentimes, I’ll hear aides use the phrases ‘my residents’ or ‘my people,’” says Joanne Labiak, MSN, CRNP, CWOCN, CWS, DAPWCA, owner of Certified Wound Care Specialists, LLC, and a Medline consultant. “There is this personal accountability. They see it as more than just a job,” she says. That’s why it’s important to truly rely on your CNAs and educate them to feel empowered to use the right products and best practices.
Provide education and training to create a culture of prevention
During the height of the COVID-19 crisis, education was challenging. At first, everything that was planned in person was canceled, from educational presentations to product demonstration fairs and workshops.
In fact, 37% of survey respondents said they’ve received less education and training on pressure injury prevention since March 2020. The survey revealed write-in comments from nurses, such as, “None. Zero. Nothing,” “I feel left out to dry,” and “Hit or miss” that starkly described their experience.
37%
of nurses said they’ve received less PI education
60%
of nurses said they prefer to learn online
41%
of nurses said they prefer peer-to-peer training
Virtual education and training soon became the norm and worked well in some cases. Many nurses who were surveyed said online classes made it convenient to attend when and where it fit into their lives. In fact, 60% of nurses said they prefer to learn online.
However, others expressed frustration with virtual learning, and 41% said they prefer peer-to-peer training.
Regardless of what kind of education nurses prefer, write-in answer feedback was loud and clear: There’s a need and desire for more education and training, but staffing shortages have made it difficult to implement. That’s why we’ve rounded up some suggestions on ways to strengthen your pressure injury prevention and training toolbox.
7 ways to help educate staff on PI prevention
How do you help make prevention education a top priority despite the challenges? Here are some do’s and don’ts:
- Do use educational packaging. Promote the use of products that include simple instructional graphics and steps. Smart educational packaging makes it easier for staff to choose the right products and apply them correctly, both of which can lead to better outcomes for your patients and residents. In one study, nurses with traditional packaging were not able to apply a dressing correctly, but 88% of nurses who used a dressing that had educational packaging were able to apply the dressing correctly.³
- Do encourage the “why.” “Nurses have to understand the why, not just the what or the how,” says Patricia Turner BSN, RN, CWOCN, CWS, Medline Director of Clinical Resources, Skin Health-Acute Care. “Why is turning and repositioning so important, why would I put on a sacral dressing, why am I going to get a patient on a support surface. Knowledge is empowerment.”
- Don’t reinvent the wheel. Use a turnkey educational program to create a Skin Champion team that helps encourage effective, systemwide pressure injury prevention.
- Do make it fun. How about some “potty talk”? Yes, that’s what one of the Medline Skin Health Advisory Board members calls the educational reminders they hang in bathroom stalls. “When the nurses go into the bathroom, there will be at least 20 seconds when they’ll be staring at the wall,” she says. “So, we took advantage of that real estate.” They also make it humorous and memorable. For instance, one of their potty posters described applying a skin barrier cream “like painting a child’s face” instead of “frosting a cupcake.”
- Don’t do it alone. Consider partnering with another clinical expert to help you and your team identify gaps and opportunities. An on-site or virtual Skin Health assessment provides customized recommendations and ongoing support.
- Do use simple decision trees. Algorithms help make complicated prevention strategies easier. For example, check out this guide to determining the right heel protection.
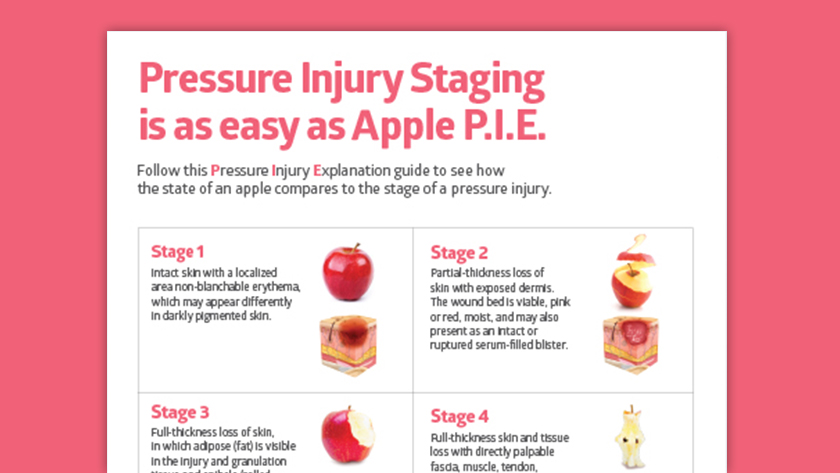
- Do use a variety of learning resources. There are amazing digital resources, including online learning opportunities, but sometimes to-the-point printed material is handy too, like a pressure injury staging poster and a guide to help distinguish incontinence-associated dermatitis from a pressure injury. One Medline Skin Health Advisory Board member chooses a monthly pressure injury prevention topic that’s discussed in huddles. Then, based on challenges nurses have at the bedside, she creates a one-page booklet with tips nurses can refer back to.
Support prevention strategies with the right system of products
A successful pressure injury prevention initiative includes evidence-based products that support best practices. Selecting products that work together as a system makes it easier for staff to know what to use when.
“Clinicians and physicians sometimes mix and match products, but they’re not tested to be used that way,” Labiak notes. She explains that a system of products pulls everything together, from education to utilization.
“Clinicians and physicians sometimes mix and match products, but they’re not tested to be used that way.”

Joanne Labiak
MSN, CRNP, CWOCN, CWS, DAPWCA
In order to gauge what products might be missing from protcols, we asked nurses what products they’re currently using to help prevent pressure injuries. Their survey answers revealed several areas that warrant improvement:
- Turning and repositioning. While close to 64% of those surveyed said they use turning and repositioning sheets, less than 50% are using wedges, and only 43% are using dry pads. Repositioning sheets, wedges and dry pads go hand in hand to help reduce risk of skin breakdown by both redistributing pressure and managing moisture. Strategies to protect fragile skin may be weakened by not using all the appropriate tools.
Case study: The impact of products on patient safety
At one multifacility healthcare organization, the Medline ComfortGlide® Turning and Repositioning System—turning sheet, drypad and wedges—was used to help reduce the risk of pressure injuries. In 2019, a decision was made to replace ComfortGlide with a less expensive alternative that included a single underpad product that was falsely positioned as a replacement for the more comprehensive system of products.
Cutting costs meant clinicians were forced to use a product that made it harder for them to do their job. The result was a 75% increase in pressure injuries. By tracking outcomes, clinicians were able to show how a return to the original ComfortGlide system of repositioning and offloading products could improve patient skin health.
Eventually, the intensive care units switched back and saw a dramatic reduction in pressure injury rates, while the non-intensive care units continued to offer the cheaper product and had a continued increase in pressure injury rates.
- Sacrum protection. An impressive 74% of survey respondents said they’re using a sacral foam dressing as part of their pressure injury prevention protocols. The flip side is that this implies that 26% of facilities are not. And that could mean that they may not be fully protecting their patients from pressure injuries at the sacrum. NPIAP guidelines recommend using prophylactic sacral dressings, specifically a soft silicone, multilayered foam dressing.²
- Daily skin care regimen. As noted earlier, 62% of nurses surveyed said they thought they should be doing more to focus on everyday skin care. Their responses to what skin care products they’re currently using support the need to improve patient and resident skin care. Only about 54% of respondents said they’re currently using skin cleanser and 57% said they’re using moisturizer. Keeping skin clean and hydrated is recommended by NPIAP to help protect at-risk skin from breakdown. Choosing a complete skin care system can make it easier for staff to choose products that cleanse, moisturize and protect people’s skin.4
Key takeaway
The pandemic has posed challenges for your prevention efforts and skin care protocols in ways you couldn’t have predicted. The Medline survey of 250 nurses shows that pressure injury prevention and education have not been top of mind since March 2020. But the survey also reveals nurses recognize there are areas for improvement. Use this opportunity to refocus on the basics of pressure injury prevention. Start with evidence-based best practices to guide your team, education and training to empower staff with knowledge, and a system of products that works together to make it easier to make skin health second nature.
References:
- Data on file.
- National Pressure Injury Advisory Panel, Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline 2019
- Kent, D. J. (2010). Effects of a Just-in-Time Educational Intervention Placed on Wound Dressing Packages. Journal of Wound, Ostomy & Continence Nursing, 37(6), 609–614. Available at https://doi.org/10.1097/won.0b013e3181f1826b
- Fletcher, J. (2015). Appropriate selection and use of barrier creams and films. Wound Essentials, 10(2), 64–68. Available at https://www.wounds-uk.com/resources/details/wound-essentials-10-2-appropriate-selection-and-use-of-barrier-creams-and-films