Fight the 4 pressure injury risk factors
Use all the right interventions to keep patients safe.

According to the National Pressure Injury Advisory Panel (NPIAP), “No other preventable event occurs as frequently as pressure injuries.”¹ They’re also the only hospital associated condition that’s been on the rise.² It’s a frustrating reality for both you and your patients.
So how do you reverse this trend and improve patient outcomes?
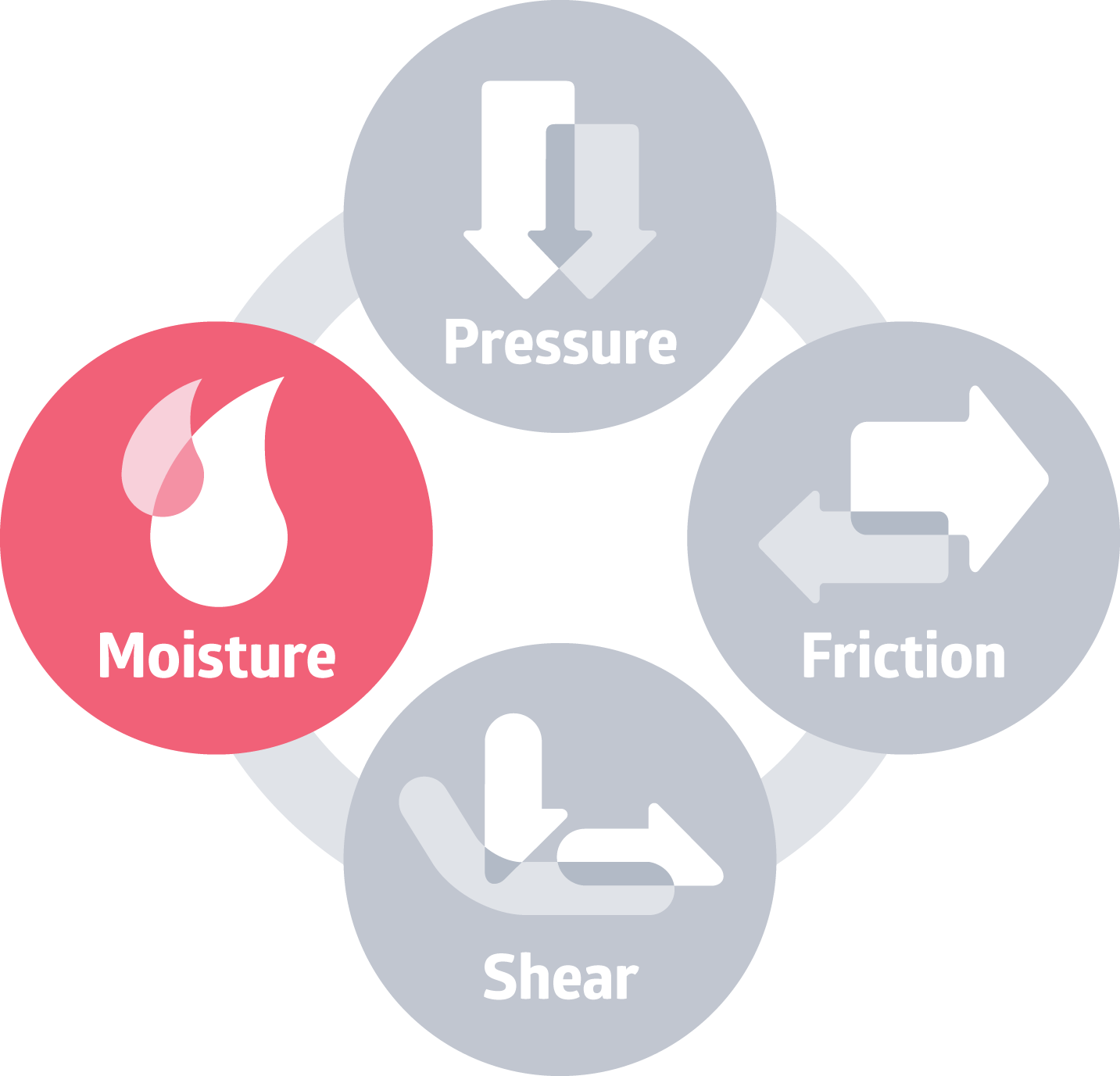
It starts with knowing the 4 main pressure injury risk factors:
• Prolonged pressure
• Friction
• Shear
• Excessive moisture
When you know the cause, you can conduct an effective risk assessment and be ready with the right interventions. In most cases, nursing assistants are responsible for providing these best practice protocols. Help educate your frontline staff to keep the 4 factors top of mind and consistently follow evidence-based best practices to help prevent tissue damage or skin breakdown.
1 | Prolonged pressure
Pressure over many areas of the body can cause skin damage. Higher risk areas include bony prominences like heels, hips and tailbone, which all have less fatty tissue. Prolonged pressure increases the risk because it can cut off blood flow to underlying tissues. Without sufficient blood circulation, cells don’t get enough nutrients and oxygen and can die.
The intervention: Reduce pressure by positioning patients at the NPIAP-recommended 30-degree angle with wedges that are easy to use and comfortable for patients. For vulnerable heels, avoid using traditional pillows that can slip and skew leg alignment. Instead, heel offloading devices are designed for management of pressure on the heel while stabilizing the lower leg. Studies show that adding prophylactic dressing at the heels can also help.
Be sure to pay extra attention to patients who are immobile or can’t easily move by themselves, such as those in surgery and with spinal cord injuries.
2 | Friction
Friction occurs when skin is dragged across a surface, such as when a patient is moving in their bed.
The intervention: Protect patients’ sacral area with a five-layer foam dressing that helps reduce friction between the skin and the surface.
Be sure to pay extra attention to bariatric patients who are often at higher risk because they may be dragging their bodies when adjusting positions or getting in and out of bed.
3 | Shear
Friction and shear go hand in hand. Shear happens when perpendicular and parallel forces work against each other, so one part of the body is pushed down, and another part is pushed side to side.
The intervention: Along with a five-layer foam dressing that can absorb shear force, use a repositioning sheet to safely and gently move patients to help redistribute pressure while in bed, as well as during transfer from one surface to another.
4 | Moisture
When it comes to reducing the risk of developing pressure injuries, it’s important to balance moisture on the skin. Too much moisture or too little can weaken the skin’s natural barrier.
The intervention: The right system of skin care products can help keep fragile skin clean and properly hydrated. When incontinence is an issue, cleanse the skin promptly with a pH-balanced cleanser after each incontinence episode and consider adding a moisture-proof dry pad to manage moisture and keep patients dry.
Plus, that same five-layer silicone dressing that helps protect against friction and shear can also help maintain skin’s optimal microclimate.
Be sure to pay extra attention to skinfolds that can get irritated from a combination of trapped moisture and friction in areas such as armpits, beneath the breasts, genital areas and skinfolds of the abdomen. An antibacterial wicking sheet can be applied to skinfolds to help manage moisture and minimize skin damage.
Key takeaway
You work hard every day to manage pressure injuries, but educating frontline staff on best practices can be challenging. Empower them with knowledge of 4 contributing factors of pressure injuries and the importance of pairing best practices with the right interventions to help improve outcomes.
Explore more content to help reduce pressure injuries:
Preventing pressure injuries: 6 best practices to improve patient outcomes
Evidence-based best practices for heels: NPIAP guidelines that help you prevent pressure injuries
Get CE credits: Skin Health and Prevention
Watch the webinar: Building a Pressure Injury Prevention Program that Works
Obesity and skinfolds: 4 proven ways to help shield patients from moisture-associated skin damage
References:
- Pressure Injury Prevention Day. npiap.com. (2019). National Pressure Injury Advisory Panel. Available at https://npiap.com/news/479002/Pressure-Injury-Prevention-Day.htm
- Hospital acquired conditions are declining—so why are pressure injuries on the rise? (2019, November 14). Advisory Board. Available at https://www.advisory.com/en/daily-briefing/2019/11/14/pressure-injury