4 essential NPIAP best practices to share with your team
Share these NPIAP best practices to reduce pressure injuries.

A 2013 Medicare study reported that the incidence of hospital-acquired pressure injuries is as high as 4.5 percent in hospitalized patients in the United States, with the care of these injuries costing an estimated $11 billion.¹
As a skin care expert, you know that pressure injuries, once referred to as decubitus ulcers or pressure sores, are an important concern for both clinical care and the healthcare system at large. Sharing evidence-based best practices with frontline staff can help reduce the likelihood of pressure injuries and improve skin and wound care all around.
4.5%
of hospitalized patients were reported to have a hospital-acquired pressure injury¹
The dedicated resource for best clinical practice guidelines is, of course, the National Pressure Injury Advisory Panel. Yet, a 2019 survey Medline conducted with 899 clinical staff indicated that there may be a lag between NPIAP guidelines and clinical practice.
For example, nearly 92 percent of those surveyed reported turning or repositioning patients every two hours2—but this is no longer the recommended process.
Pressure injury prevention protocols to know
Many pressure injuries may be preventable with the right practices, including proper turning and repositioning, moisture management, heel offloading3 and consultation with a clinical partner.
Below you’ll find key NPIAP-recommended best practices to share with your frontline staff that can help reduce pressure injuries.
Know the 4 main contributing factors of pressure injuries: Download this poster to share with staff.

1
Proper turning and repositioning to keep skin healthy
Previous NPIAP guidelines recommended turning patients every two hours to treat or prevent pressure injuries. But newer research has changed that.
According to the most recent NPIAP Clinical Practice guidelines, updated in 2019, the frequency of turning and repositioning patients should be determined individually by a patient’s activity level and ability to reposition themselves.4 Using the right repositioning system to help reduce pressure and safely and gently move patients.
Tip: Clinicians should take into consideration a patient’s overall medical condition, skin and tissue tolerance, pain tolerance and overall treatment objectives.
Does your staff know the updated guidelines?
In 2019, Medline conducted 48 Skin Health Solution Discovery Assessments, which included a survey of 899 clinical staff at acute care facilities. Insights from the survey indicate that frontline staff may need additional education and training on updated NPIAP guidelines.2
56% of staff do not have a usage protocol in place for sacral foam dressings as part of a pressure injury prevention program.
91% of staff report turning or repositioning patients every two hours, which is no longer the NPIAP recommendation.
65% of staff would like more training in pressure injury staging.
40% of staff report using heel protector devices (bunny boots, heel pads) for offloading heels.
42% of staff report that they don’t apply daily moisturizer on patients.
Read the full report of our findings. Download the white paper now.
2
Manage moisture to protect fragile skin
Skin that’s too dry or too moist can be one of the significant risk factors for pressure injury formation. NPIAP notes that skin should be kept clean of excessive moisture and appropriately moisturized, following a daily skin care regimen.4
Tip: Patients with incontinence are prone to developing pressure injuries, so be sure to apply a barrier cream after cleansing.4
How can sacral foam dressings help?
The most severe pressure injuries occur at the sacrum 44.8% of the time.4 NPIAP Clinical Practice guidelines recommend applying a sacral foam dressing to reduce the likelihood. If you don’t have them already, implement protocols that include regular use of five-layer sacral foam dressing on higher-risk patients. This practice can help manage friction, shear and excess moisture that can contribute to pressure injury formation.
3
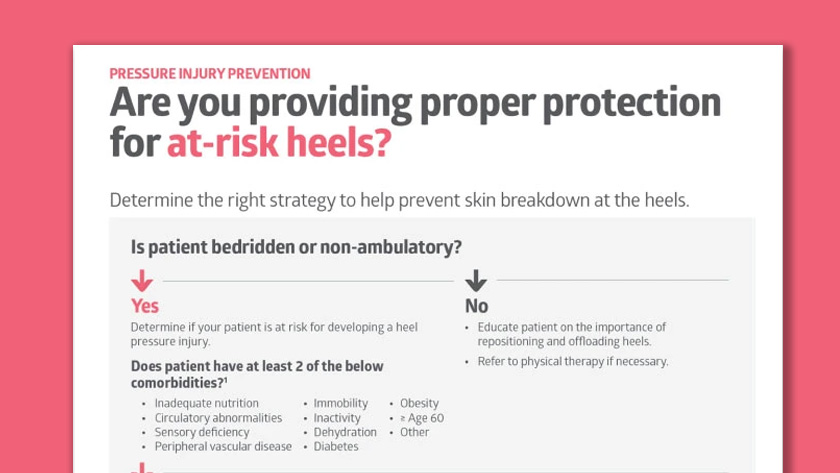
Relieve pressure at the heels
The NPIAP recommends elevating the heels with a heel offloading device. Be sure to encourage this practice with patients at risk of heel pressure injuries, as well as patients with existing stage I or II heel pressure injuries.5 Heel offloading can decrease the length of hospital stays and promote patient ambulation by preventing heel pressure injuries.5
Tip: Avoid using traditional pillows or foam cushions to support the heel, which can slip and get out of alignment.
4
Engage a clinical consultant to help identify gaps and opportunities
Around 60,000 people die every year from complications associated with pressure injuries.5 Preventing pressure injuries is a multifaceted goal that includes best practice guidance, education and training, and the right system of products. The findings from a series of Medline Skin Health Solution discovery assessments indicate that there is room for improvement.
With pressure injuries at such high rates, it’s important to stay on top of prevention best practices. An experienced clinical consultant can help. Through a detailed discovery assessment led by a wound care expert, you can better identify variations in care and then help educate staff in best practices for promoting skin health.
Key takeaway
Help reduce skin breakdown by educating frontline staff on the most updated NPIAP-recommended evidence-based best practices. You can help reduce hospital-acquired pressure injuries with the right protocols in place for turning and repositioning patients, protecting the sacrum, offloading heels and following a skin care regimen for moisture management. A clinical consultant can help you identify opportunities to standardize care and further educate staff.
References:
- Truang, Bao, et al. “Pressure Ulcer Prevention in the Hospital Setting Using Silicone Foam Dressings.” Cureus, vol. 8, no. 8, 2016, pp. 1–6
- Data on file
- Boyko, Tatiana, et al. “Review of the Current Management of Pressure Ulcers” Advances in Wound Care, 7, no. 2, 2018, pp. 57–67
- Haesler, Emily, et al. European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline. The International Guideline
- Al Aboud, Ahmad, and Biagio Manna. “Wound Pressure Injury Management”