Nursing onboarding process: 10 tips to maintain care quality
Build teamwork and keep skin health best practices top of mind.

It’s no secret that there’s been a growing nurse shortage over the past decade or two, and COVID-19 only accelerated that trend. One survey revealed that some hospitals have lost up to 30% of their permanent staff due to factors related to the pandemic.¹
30%
of permanent staff have left some hospitals¹
Now, healthcare facilities are tasked with filling their nursing gap—in any way they can. Strategies have included calling retired nurses back to work, pulling full-time nurses to cover unfamiliar units, scouting nursing school graduates, and hiring per diem, contract, international, and travel nurses. In fact, some reports say travel nurses currently make up as much as 10% of a hospital’s staff.²
What’s your role in this? As the default skin and wound care expert, it likely falls to you to get new nurses up to speed quickly and empowered with the right tools and strategies to care for patient skin.
Although this ever-changing landscape can seem challenging, it also presents you with new opportunities to target skin health and pressure injury prevention in different, and maybe even better, ways. Make onboarding easier with this checklist of 10 skin health essentials, compiled with help from Medline Clinical Education Specialist Dr. Doreen Gendreau.
1
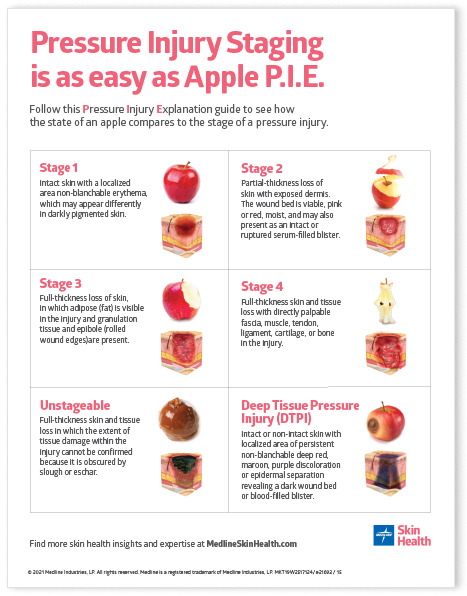
Inform everyone on the basics of pressure injury staging
Give nurses simple ways to identify pressure injuries so they know the right interventions and treatment. Our popular Apple P.I.E. poster is a handy visual reference. Download the Apple P.I.E. poster now.
2
Highlight the importance of thorough skin assessment documentation
Preventing and healing wounds calls for comprehensive skin assessments and meticulous documentation. Be sure to arm any new staff with your facility documentation requirements and guides so your patient gets the best care and Medicare gets the right information.
3
Encourage staff to use the Braden Scale consistently
The Braden Scale is an important tool for identifying a person’s risk of developing a pressure injury. Have printed copies available and try to find time for a quick review.
4
Ensure caregivers apply products correctly
While you may know how to apply that heel boot or sacral dressing, you don’t know the experience level of an incoming nurse. Encourage them to take advantage of educational packaging and direct them to useful how-to application videos.
5
Make sure everyone knows their role and responsibility
Create or provide an updated organizational chart that spells out who does what when. For instance, will the travel nurse need a consultation to stage a pressure injury? Do they take wound photos? If not, who does? When are supervisors called versus managers?
6
Define when and how to share patient information across teams
To make the patient journey between different care areas as seamless as possible, be sure everyone—especially new or travel nurses—knows what information needs to be shared from one step to the next.
7
Point out all product locations
Get specific in terms of where new nurses and travel nurses can find the products they need, so they’ll be able to quickly access supplies. Do you use a system of products that work together? If so, note that too. For example, a ComfortGlide™ bundle typically includes a repositioning sheet, drypad and two wedges, so be sure they know where to find each of these items. You might even create a layout of the units, indicating where each supply area is located.
8
Provide a directory of important contacts
Learning a lot of new faces and names can be stressful for new nurses. Give them a cheat sheet of essential colleagues, complete with headshots, name pronunciations, titles and contact information.
9
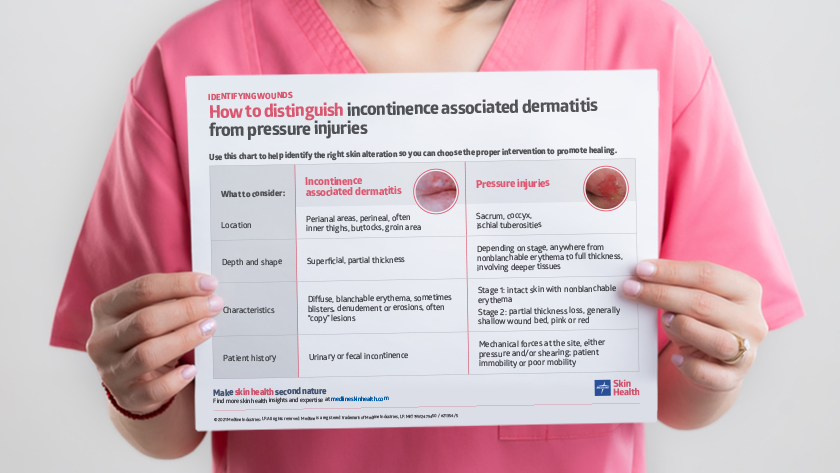
Suggest additional educational resources
Ideally, every new nurse or travel nurse would take on a Skin Champion role, but that’s not possible when they’re focused on other priorities or only at your facility for a short time. But you can still help them find learning opportunities, such as skin health webinars, online classes and other skin and wound care content.
10
Make the most of your clinical partners
Look to other clinical experts and resources to help you streamline your onboarding process. For example, Medline’s Skin Health Solution provides best practice guidance, education and training, and systems of products that support your skin health initiatives. See how it can help you.
Key takeaway
The ongoing national shortage of nurses and persistent staffing challenges has led to outside-the-box thinking in order to continue to provide the best care for patients. The use of travel nurses and agencies to provide that care has become mainstay during the pandemic. While this may lead to some frustration and stress among permanent nursing staff, it also gives you the chance to create a more positive experience. Empower more skin health allies by being prepared with the right tools, resources and education. Start with the list of 10 essentials above and learn how Medline clinicians can help you make skin health second nature for everyone.
References:
- Muoio, D. (2021, April 20). “Hospital executives report high nursing vacancies, greater reliance on costly travel nurses.” FierceHealthcare. Available athttps://www.fiercehealthcare.com/hospitals/hospital-executives-report-high-nursing-vacancies-greater-reliance-costly-travel-nurses
- Bernstein, L. (2021, December 6). “As covid persists, nurses are leaving staff jobs — and tripling their salaries as travelers.” Washington Post. Available at https://www.washingtonpost.com/health/covid-travel-nurses/2021/12/05/550b15fc-4c71-11ec-a1b9-9f12bd39487a_story.html