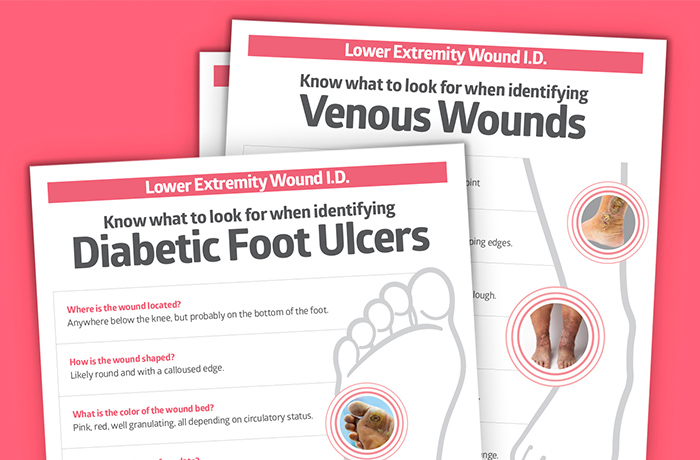
Diabetic foot ulcers vs. venous or arterial ulcers: 3 posters
Help staff distinguish common lower extremity wounds to determine best care.

In the United States, it’s estimated that up to 13 percent of the population has a lower extremity wound of some kind. Together, they cost the healthcare system more than $20 billion.¹ The three most common of these chronic wounds are diabetic foot ulcers, venous ulcers and arterial wounds.
Up to 5%
of Americans over 80 have a lower extremity wound¹
2.5
million Americans will develop venous ulcers each year¹
25%
of diabetics will get a diabetic foot ulcer in their lifetime¹
Distinguishing lower extremity wounds can sometimes be challenging for frontline staff, because characteristics may seem similar. The right care and management of lower extremity wounds starts with knowing how to properly identify them. That’s why we created these three educational posters to share with staff and provide some key differences and typical management strategies below.
Venous leg ulcers
Overview: Venous leg ulcers occur most often on the medial lower leg and are usually a symptom of venous disease. Problems with blood flow in the veins of the legs can cause abnormally high pressure, leading to capillary leakage and skin breakdown.
How to manage VLUs: Treatment therapies focus on compression. Which type of compression product you choose will depend on the purpose of your compression solution—for instance, if there’s wound drainage, you might want a four-layer compression product in combination with a contact layer or primary non-adherent dressing, as appropriate; or maybe you’re recommending a garment that’s easy for patients to use at home.
Learn more about which compression product is right for your patient.


Arterial wounds
Overview: Arterial wounds, often caused by peripheral arterial disease (PAD), are the second most common type of lower extremity wound. You’ll tend to see this more in patients over 50 and with a history of smoking, hypertension or heart disease.²
How to manage arterial ulcers: These types of lower extremity wounds are generally caused by a lack of blood flow and oxygenation to areas farthest from the heart, including the toes and the front part of the foot.¹ The diminished blood supply leads to cell death and skin damage. Look for these wounds on the distal part of the limb, often on the foot, at the tips of toes or in between toes.

Treatment for arterial wounds can be complicated by factors such as the stage of the disease and the extent of the damage. Start with wound bed preparation with a dressing that promotes moist wound healing.³
The underlying problem of circulation may require a surgical solution, so it’s important to rely on a multidisciplinary team to help determine the best approach.
Diabetic foot ulcers
Overview: About 25 percent of patients with diabetes will develop a foot ulcer at some point.¹ These wounds are most often located on the bottom of the foot and often caused by the presence of angiopathy and neuropathy. Angiopathy leads to abnormal blood flow to the extremity. Neuropathy can cause a lack of sensation to the foot, which could result in trauma and injury. Another contributing factor is the abnormal response diabetics may have to infection.4
How to manage DFUs: Diabetic foot ulcers can be managed with offloading devices, as well as gentle debridement of devitalized tissue. Help protect at-risk skin from fissures and cracking that can contribute to skin damage by applying moisturizing skin care that smooths and conditions severe dry and scaly areas of the foot.

Key takeaway
Lower extremity wounds can be difficult to manage. The best place to start is by learning how to identify each wound correctly. Then follow up with the best practices and products to help your patients’ wounds heal. Download these educational posters to help empower staff to sharpen their wound care expertise.”
Learn more about managing lower extremity wounds:
Venous leg ulcers: 4 ways to help improve patient compliance and quality of life
Diabetic foot ulcers: a podiatric surgeon’s perspective on chronic wound management
How do you distinguish a venous ulcer from an arterial wound? Here’s your guide
Management of chronic wounds: Chronic wounds are chronic infections caused by biofilm
Take a Medline University course: The Management and Treatment of Arterial and Diabetic Neuropathic Wounds
References:
- Star, A. (2018). Differentiating Lower Extremity Wounds: Arterial, Venous, Neurotrophic. Seminars in Interventional Radiology, 35(05), 399–405. Available at https://doi.org/10.1055/s-0038-1676362
- Vera, M. (2017). The Challenge of Lower Extremity Wounds – Arterial Wounds, Part 2. WoundSource.Com. Available at https://www.woundsource.com/blog/challenge-lower-extremity-wounds-arterial-wounds-part-2
- Hopf, H. W. (2006, November 1). Guidelines for the treatment of arterial insufficiency ulcers. Wiley Online Library. https://onlinelibrary.wiley.com/doi/10.1111/j.1524-475X.2006.00177.x
- Yazdanpanah, L. (2015). Literature review on the management of diabetic foot ulcer. World Journal of Diabetes, 6(1), 37. Available at https://doi.org/10.4239/wjd.v6.i1.37