Healing diabetic foot ulcers: Real-life wins using PluroGel

A 42-year-old man with a chronic diabetic foot ulcer entered the office of Dr. Brian Lepow, DPM, a board-certified, surgically trained podiatrist, Assistant Professor of Surgery at Baylor College of Medicine, and a Medline consultant. The wound wasn’t infected, Dr. Lepow explains, but it was heavily necrotic and fibrotic. He applied PluroGel Burn and Wound Dressing and, after only a week, Dr. Lepow remarks, “I couldn’t believe how improved the wound was.”
Chronic wound stories like the one above have led Dr. Lepow to recommend PluroGel to his fellow colleagues, including vascular surgeons and podiatrists. “When I become impressed with something, I become very passionate about it and want other people to know and realize that there are better ways to manage these patients,” says Dr. Lepow, who sees about 80 to 100 patients a week in his multidisciplinary clinic located in the department of vascular surgery and focuses on limb preservation.
How PluroGel helps manage chronic wounds
PluroGel is a concentrated surfactant-based burn and wound dressing. Through its unique micelle matrix technology, it does three main things to help manage chronic wounds:
1. Removes barriers to healing.
2. Creates a moist wound environment.
3. Shown to disrupt and prevent biofilm in vitro.¹
We had a chance to speak with Dr. Lepow about his experiences with PluroGel and how it has helped his patients’ diabetic foot ulcers improve and, in some cases, avoid lower extremity amputations.
Q: How did you get introduced to PluroGel?
Answer from Dr. Lepow: I was introduced to PluroGel when I started my limb salvage practice. I’m always looking for alternatives to how I can better manage my patient population. I feel it’s always my job to see what’s out there, and it’s important to try everything. I’ve been using PluroGel for about three years now. It was a no-brainer for us to explore a new solution and easy to work into my practice.
Q: You’ve done some evaluation of PluroGel. What were your first thoughts about it?
Answer from Dr. Lepow: I started some basic utilization in the clinic and saw some fairly instantaneous and very impressive results. This was with patients who had chronic diabetic foot ulcers, had used alternative therapies and didn’t make a lot of progress. What was really interesting to me was that, after a week of using PluroGel, there was significant reduction in the fibrous tissue in the wound beds in a lot quicker manner. From there, I really became an avid user of it and, not only that, but an advocate in our hospitals.

“It was a no-brainer for us to explore a new solution.”
Q: Were you able to evaluate PluroGel in a measured way?
Answer from Dr. Lepow: I’ve done a small series case study. I have a few cases where patients are seeing me as second or third consultation, so they’ve tried everything else, and when I can put something on that makes a big difference, sometimes within a week’s time period, that’s great. Patients are healed faster, they go into diabetic foot remission and are seen to have more ulcer-free days, which is everything we strive for with our patient population.
Q: How does PluroGel compare to other products you’ve tried?
Answer from Dr. Lepow: PluroGel is really a novel product, there’s nothing else like it out there on the market. I think it shortens duration of use, I think it’s easier to obtain, more cost-effective for patients, and you don’t get as many side effects as with other products. Some of my patients who were using some of the alternative products were getting burning and maceration around the periwound space—a lot of those things that really became problematic and thus not friendly for the tissue.
Learn more about the innovative science behind PluroGel
Q: How have patients responded to PluroGel?
Answer from Dr. Lepow: Patients are happier. Of course, if I can keep them out of the OR that’s great, that’s a win. In fact, in some cases patients have come in expecting to have surgery, and using PluroGel has reduced the need for surgical intervention. It performs the act of cleaning, trapping and removing debris from wound.
Q: How do your colleagues like PluroGel?
Answer from Dr. Lepow: Those in the hospital, including the WOCNs who see 30 to 50 patients a day, all echo the sentiments that PluroGel is a great product, they love it, they use it all the time, and I’ve really seen a change in how they practice.

Q: You brought it to their attention?
Answer from Dr. Lepow: Yes, when I started here, it was my goal to function as a team, and some of that includes working closely with our WOCNs, because they do a lot of the wound management. I like to meet with them quarterly, check in with them, find out where they have an unmet need and how I can help. That’s kind of where PluroGel came about. This was in the early stages of my introduction to PluroGel. I told them what my experience was and suggested they try it. They’ve really taken a liking to it.
They see that I’m doing something different, and they’re interested to find out why my cases more successful, why are my length of stays shorter. I think because of that, they’re more open to talking about new things that are out there and ways to better manage wounds.

Week 1: Initial presentation
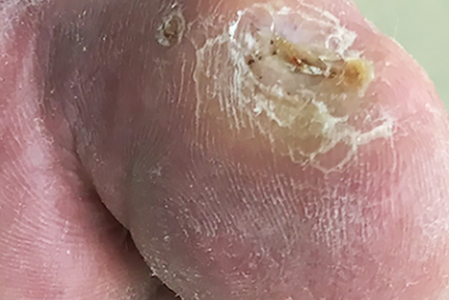
Week 10: Healed
Q: Can it be challenging to get people to change the product they’re used to?
Answer from Dr. Lepow: Absolutely, that’s a huge problem. For the hospitals to have buy-in—to convince a hospital to buy something new and buy less of something they’ve been familiar with—I deal with that all the time. But I don’t bring in a product for any other reason than it’s working well for my patients. If it’s a great product, and I think it’s doing a good job, I’m going to talk about it and tell people about it.

“Patients… are seen to have more ulcer-free days.”
Q: If you were telling a peer about PluroGel, what aspects would you highlight? Debridement? Biofilm? Patient reported pain?
Answer from Dr. Lepow: I turn to PluroGel for all of the above. I use it as a debridement agent. I use it for reduction or removal of biofilm. I’ve used other therapies in the past that patients reported were painful and burning. Or they’ve been using those other products for a number of months and haven’t had any improvement. Honestly, PluroGel is top on my list to use for chronic wound management.
463 million
adults have diabetes worldwide²
More than 80%
of amputations begin with foot ulcers²
Q: Is there a point at which you say a diabetic foot ulcer is a limb-threatening concern? Or is every DFU a potential limb-threatening concern?
Answer from Dr. Lepow: Every patient who walks in the door that has a chronic diabetic foot ulcer is at risk for losing a toe, a foot or a leg. I have that conversation with those patients pretty much from day one, and I revisit that conversation as frequently as I can, because I think the statistics show that once you have a diabetic foot ulcer, the mortality rate is pretty high, and your risk for amputation is there.
I don’t want to scare patients or family, but I want them to understand the reality: if you don’t take care of a small ulcer, it can develop into something very serious very quickly, and we see that all the time. A lot of it is poorly controlled diabetics and noncompliance. Patients often think, ‘Oh well, let’s give it a few more days, see if it gets better,’ and that usually doesn’t end well.

Week 1: 0.5cmx0.5mx0.1cm

Week 2: 0.2cmx0.2vmx0.0cm

Week 4: Healed
Q: Is there a particular sweet spot where you see PluroGel working best, such as a tissue type or wound type?
Answer from Dr. Lepow: I do have a growing population of patients that have fairly serious vascular disease and have painful arterial ulcers that really can’t be managed in the OR because they’re too sick—that’s a great population for PluroGel. I also have patients who have chronic, non-healing wounds and we can’t seem to get them over the hump to closure, so I’ve used it for that population as well.
Any patient that comes in with a wound that has slough or fibrotic tissue to it, it’s definitely, 100% a go-to solution for me. It’s making a difference for my patients.
With the number of people with diabetes continuing on the rise, diabetic foot ulcers have become a growing concern for podiatric surgeons and wound care professionals. When chronic DFUs are not managed properly, it can increase the risk of amputation. It’s important to know what products can help you efficiently and effectively address these types of wounds. PluroGel can help you by removing barriers to wound healing, creating a moist wound environment, and disrupt biofilm (based on in vitro testing).¹
More resources to help you manage diabetic foot ulcers and other chronic wounds
Watch how PluroGel works to help manage chronic wounds
Discover more about PluroGel’s unique surfactant-based formula
Learn more about treating diabetic foot ulcers
Download a poster to help identify a diabetic foot ulcer
References:
- Yang Q, Larose C, Porta AD, Della Porta AC, Schultz GS, Gibson DJ. A surfactant-based wound dressing can reduce bacterial biofilms in a porcine skin explant model. International Wound Journal. 2017;14(2):408-413
- Avoiding amputation: Jump feet first into diabetes foot care. (2020, September 23). Retrieved January 29, 2021, from https://www.mayoclinic.org/diseases-conditions/diabetes/in-depth/amputation-and-diabetes/art-20048262