Debridement: What clinicians need to know
Your guide to this essential part of wound management.

How confident do you feel about wound debridement? It’s common to feel uncertain about these procedures. Yet, as a clinician on the fronlines, you provide the majority of wound care. That’s why it’s helpful to get up to speed on debridement and start incorporating it into your practice.
You don’t need to know how to perform every procedure to help your patients and put stalled and chronic wounds on the path to healing. You can help by having the knowledge and skills to:
- Accurately assess wounds and know when to debride
- Understand the best methods for different wound types
- Factor patient history and adherence into the choice of procedure
Topics covered:
INTRODUCTION | INDICATIONS | TECHNIQUES | FAQ
What is debridement?
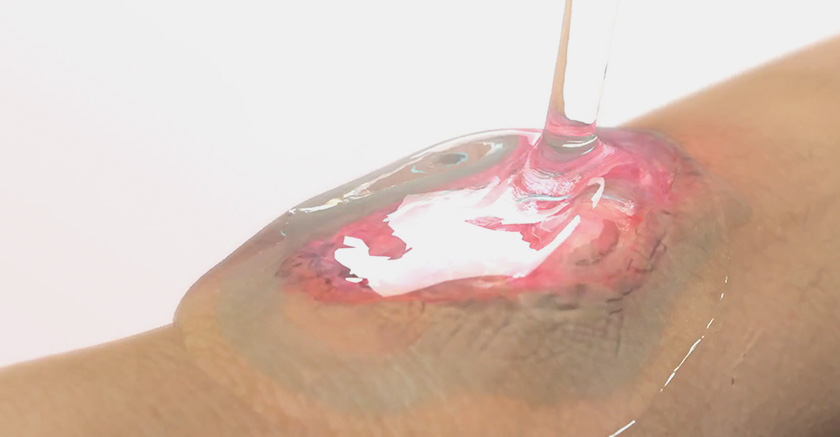
Debridement, a standard in wound management, involves the removal of the nonviable tissue that delays wound healing. During these procedures, a range of techniques are used to remove the dead or contaminated tissue from the wound.
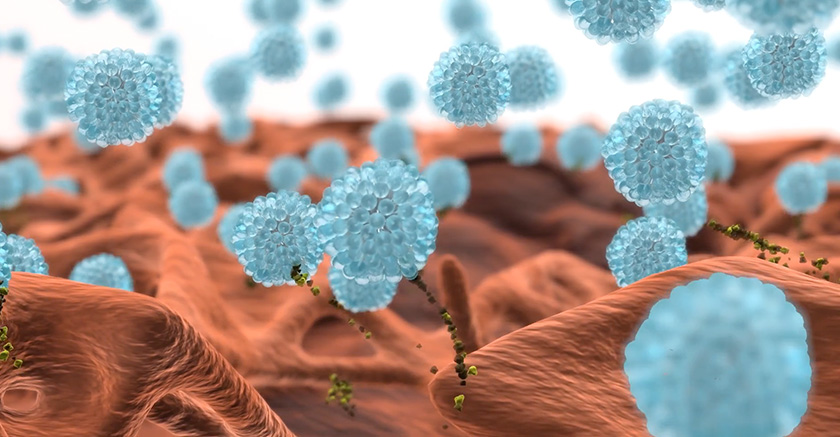
When this tissue is removed, it reduces the bacterial burden within the wound. Reducing the bioburden and presence of biofilm is key. This reduction helps stimulate the formation of granulation tissue—the tissue that signals the wound is healing—in the wound bed.
The body has a natural method of debridement called autolysis. When an acute wound enters the inflammatory state of healing, the body prepares the wound bed to allow healing to occur. During this natural process, neutrophils and macrophages clear out devitalized tissue and cell debris.
In a chronic wound, this process is delayed when damaged cells release increased levels of endotoxins. However, if the proper procedure is performed early in the process, it’s possible to overcome these barriers to healing. The appropriate intervention provides a foundation for tissue growth and accelerates the healing process.
Debridement is different from wound cleansing, which involves the removal of metabolic waste, dirt or foreign material.
Debridement is different from wound cleansing, which involves the removal of metabolic waste, dirt or foreign material.
Wound assessment
Frontline clinicians are the primary point of care for most patients with a non-healing wound. That means you have an important role to play in assessing when debridement is necessary, which method to use and when to refer a patient to a specialist.
Making those determinations starts with a structured, holistic wound assessment. As part of the diagnostic process, consider the:
- Underlying conditions that caused the wound or delayed healing
- Location, size and exudate level of the wound
- Condition of the wound bed and periwound skin
- Realistic goals for wound care
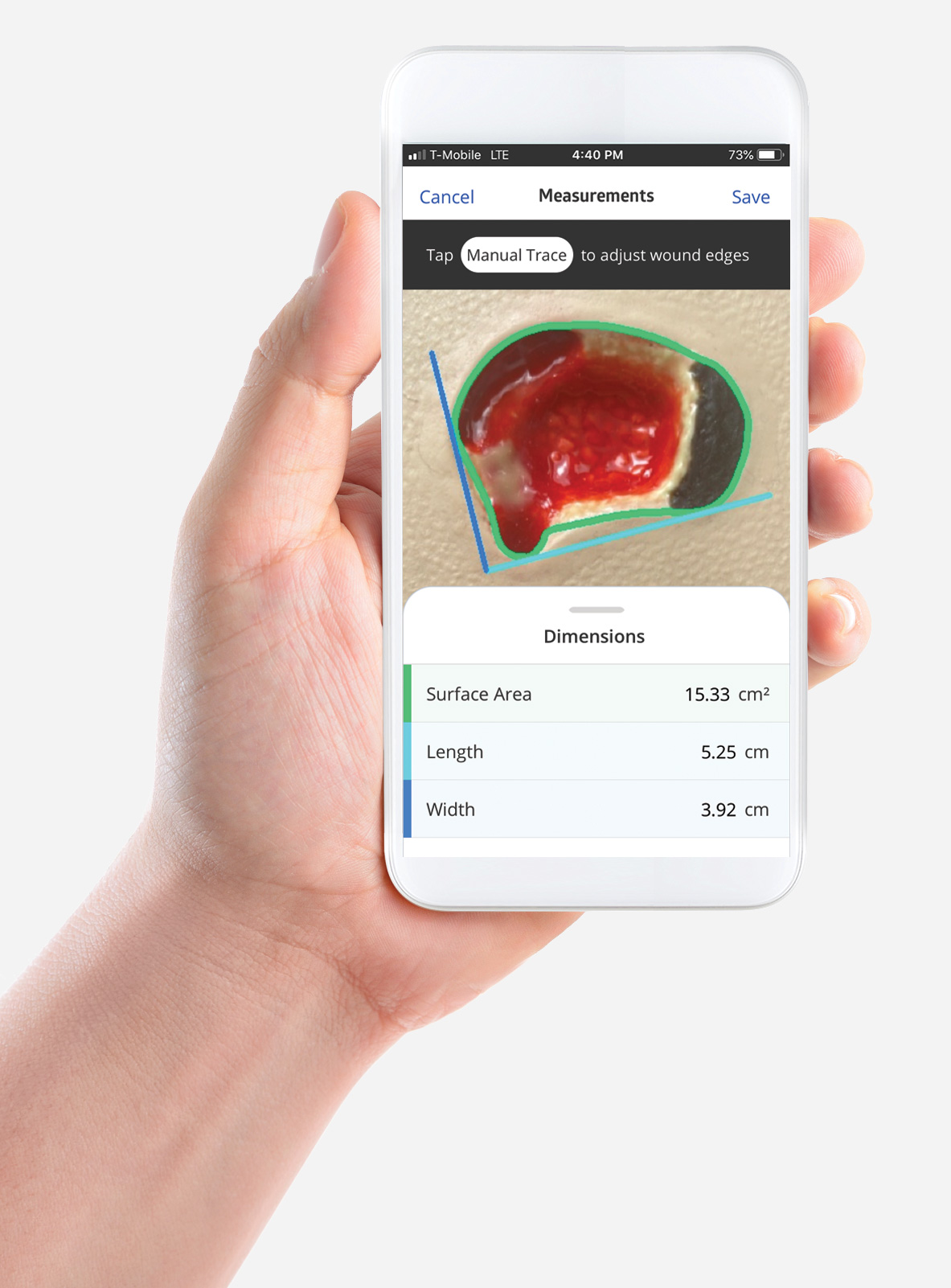
Discover the digital tool that simplifies wound assessment.
Most nonhealing wounds will benefit when you select the appropriate method. There are a select few cases where it could harm the patient. For patients with peripheral arterial disease who develop distal gangrene, debridement could put them at risk of amputation. These patients should be referred to a specialist vascular team.
When to debride?
The clearest indicator of when to debride is the type of tissue in the wound bed. If there is evidence of nonviable tissue, such as necrotic tissue, slough or eschar, debridement is an appropriate choice.
These procedures can benefit patients with pressure injuries. When nonviable tissue is removed from the wound bed, it’s easier to accurately stage these painful wounds. Why? It improves your ability to see the depth and condition of the wound bed.
Types of debridement
Currently, there are five methods:
Enzymatic/chemical
Autolytic
Mechanical
Biological
Surgical/sharp
Often the condition of the wound will determine which method or combination of methods is selected. Caregivers also consider the patient’s pain tolerance, resources and environment. The goal is always to provide the best outcome for the patient.
Debridement is commonly performed over a couple of weeks.
Chemical debridement
Also called enzymatic debridement, this process uses a synthetic chemical enzyme to break down and remove dead and damaged tissue. Chemicals such as histolyticum, collagenase, papain, varidase and bromelain are commonly used to dissolve this nonviable tissue. Doctors are selective about recommending this method because it can put viable skin at risk.
Pros:
• Some chemical agents work fast
• Low risk to healthy tissue when used properly
Cons:
• Can be expensive compared to other methods
• Need the skills to ensure that healthy tissue does not come into contact with the chemical agent
• Cannot be used on heavily infected wounds
• Avoid use on patients with known sensitivity to product’s ingredients
• May require a secondary dressing for exudate control
• May cause patient discomfort, including a burning sensation and wound pain
Autolytic debridement
Autolytic debridement uses a moisture-retaining dressing to help the body’s enzymes and natural fluids soften old tissue. This gentle procedure causes moisture to accumulate, leading non-viable tissue to swell up and separate from the wound.
It can be used on any burn or chronic wound that has noticeable wound debris, slough and nonviable tissue. Noninfected wounds and pressure injuries are ideal for this debridement process, but it should be avoided for immunocompromised patients.
Clinicians use dressings such as honey, hydrogels, hydrocolloids and hydrofibers to facilitate debridement by maintaining a moist wound environment. These dressings help create an optimal healing environment that encourage the body’s natural fluids to debride the wound. If there’s not a significant reduction in the amount of necrotic tissue within one to two days, it’s time to consider a different method.
Pros:
• Gentle
• Relatively low cost
Cons:
• Not recommended for infected wounds
• Some products sting when first placed in the wound bed
• Certain dressing types put periwound skin at risk for maceration
• May not be a good choice for high drainage wounds
• Cannot be used on immunocompromised patients or patients with poor blood flow
“Clinicians tell us that they see faster healing times when they use a surfactant-driven debridement method.”
Bridget Dever
Senior Product Manager at Medline Industries
How surfactant dressings promote autolytic debridement
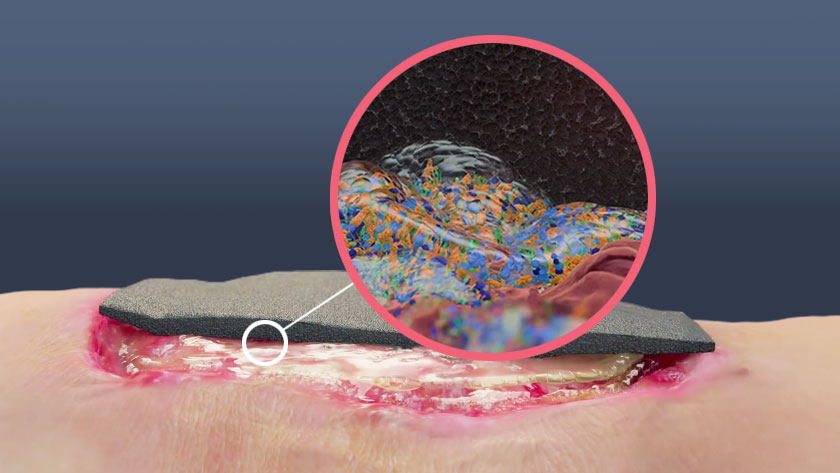
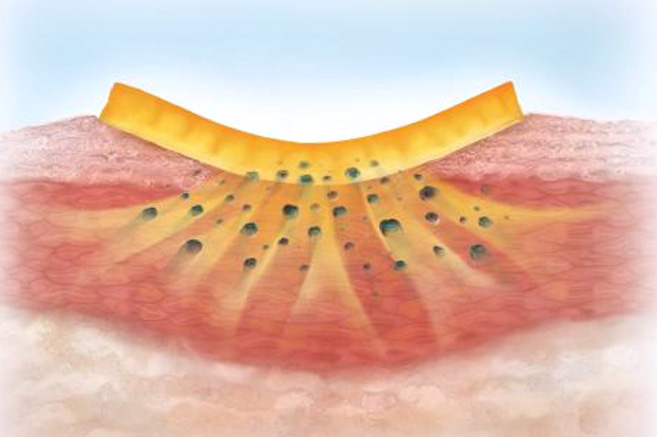
 There’s one autolytic method that won’t macerate skin around the wound: surfactant-based gel dressings. This subcategory of autolytic debridement uses a dressing with a high concentration of surfactant micelles. When the dressing comes into contact with the wound bed, the micelles link to form a matrix that expands and contracts continuously. This results in a cleansing and rinsing action that softens, loosens and drives slough and necrotic debris away from the wound bed.
There’s one autolytic method that won’t macerate skin around the wound: surfactant-based gel dressings. This subcategory of autolytic debridement uses a dressing with a high concentration of surfactant micelles. When the dressing comes into contact with the wound bed, the micelles link to form a matrix that expands and contracts continuously. This results in a cleansing and rinsing action that softens, loosens and drives slough and necrotic debris away from the wound bed.
 As Medline Clinical Manager Anita Meador, BSN, RN-BC, CWCN, COS explains it, “Surfactant-based debridement is kind of like cleaning a dirty lasagna pan.” When the pan is soaked in sudsy water, it’s easier and faster to clean. Surfactant micelles work just like this sudsy water.
As Medline Clinical Manager Anita Meador, BSN, RN-BC, CWCN, COS explains it, “Surfactant-based debridement is kind of like cleaning a dirty lasagna pan.” When the pan is soaked in sudsy water, it’s easier and faster to clean. Surfactant micelles work just like this sudsy water.
Surfactant dressings remain in gel form for up to three days, and they won’t overrecruit moisture to the wound bed. This creates an ideal moist environment that promotes timely wound healing.
Pros:
• No risk of maceration or harm to healthy tissue
• Gentle application and removal, which promotes patient comfort and adherence
• Remains in gel form for up to three days
• Doesn’t require special training or skills to perform
• Some clinicians report that it works faster and notice less wound odor
Cons:
• Cannot be used on high-exudate wounds
• Avoid use on patients with known sensitivities
Mechanical debridement
This method involves the removal of devitalized tissue using a mechanical force, and there are several techniques that clinicians use to achieve it.
Hydrotherapy: This technique uses running water to wash away non-viable tissue.
Hydrosurgery: A high-pressure stream of water removes burnt skin with this debridement type, leaving behind the healthy tissue.
Wet-to-dry dressing: With this method, wet gauze is applied to the wound. Once it dries, it sticks to the wound. When the dressing is removed, it pulls away old tissue. This method is no longer recommended because the dressing changes can be painful and strip away healthy tissue.
Monofilament debridement pads: A soft polyester pad is gently brushed across the wound during this form of mechanical debridement, removing dead tissue and debris.
Each technique has its own unique risks, but generally, these procedures have a higher risk of bleeding for patients. It’s best for acute and chronic wounds with moderate to high amounts of dead tissue, and it can be used on infected or noninfected wounds.
Pros:
• Can be used on infected or noninfected wounds
• Can be combined with autolytic to mitigate tissue damage and slow healing
Cons:
• Wet-to-dry method may reopen healing wounds and strip away healthy granulating tissue
• Painful removal
• Relatively slow process
Biological debridement
Larval or maggot therapy is a common form of biological debridement. During this procedure, sterile larvae (maggots) from the green bottle fly are applied to the wound bed. The maggots eat the dead tissue, which helps accelerate wound healing. These insects control infection by releasing antibacterial substances and eating harmful bacteria.
Sometimes the maggots are in a mesh bag, which is kept in place over the wound using a dressing. The maggots are replaced twice a week.

Pros:
• Good alternative for patients who can’t undergo surgery due to medical conditions
• Beneficial to patients infected with antibiotic-resistant strain of bacteria or large wounds
• Maggots can judge necrotic tissue with more precision than the human eye
Cons:
• Organisms can be challenging to locate
• Can be painful
Surgical/sharps debridement
Sharps debridement uses tools such as scalpels, Metzenbaums and curettes to remove devitalized tissue. This technique can be combined with different forms of debridement during the perioperative period. It’s often not a first choice and is reserved for times when other methods don’t work. The method is also a good option for wounds that are deep, large and painful or in cases where urgent treatment is necessary.

It’s helpful for clinicians to consider the patient’s surgical risk and the best setting for the procedure. They factor in how adequate the anesthesia is and how well perioperative complications like bleeding can be managed.
Pros:
• Can be performed in a doctor’s office, wound care center, operating room or bedside
Cons:
• Risk of bleeding
• Risk of complications from anesthesia
• Cannot be performed on an intact eschar (usually occurs on unstageable pressure injuries at the buttocks, heels or sacrum with intact, dry eschars)
• Can only performed by a skilled, qualified and licensed healthcare professional
Common questions about wound debridement
- What is the nurse’s role in debridement?
- It’s helpful for all nurses have competency in wound assessment to determine if debridement is necessary, the best method to use for the wound type and whether they can conduct the procedure or need to refer the patient to a specialist.
- Can nurses do wound debridement?
- It is within the practice of a nurse to perform certain types of debridement. Autolytic debridement does not require specialized skills to perform. With the proper certification, coursework and supervision, nurses can safely conduct more complicated procedures such as surgical debridement. Check your state licensing board’s requirements for each debridement method.
- What are the 4 types of debridement?
- Autolytic, surgical, mechanical and chemical/enzymatic are the four most commonly used methods of debridement. The fifth method, biological debridement, is less common.
- Does wound debridement hurt?
- Surgical and mechanical debridement can be painful, and pain control is essential with either procedure. There may be some pain with associated with each technique. Autolytic and chemical/enzymatic are less painful, and surfactant-driven autolytic debridement is remarkably gentle.
Key takeaway
As a clinician, you’re on the front lines of wound care. While you don’t need to be able to perform every debridement procedure, you can elevate the care you provide by familiarizing yourself with the different types. With the right skills and knowledge, you can assess wounds, determine care aims and select the most applicable debridement type.
This will help your patients’ wounds heal faster, eliminate unnecessary pain and reduce costs. If you want more information about chronic wounds and debridement products, visit our Skin Health website.