Dark skin tones: 6 tips to improve skin and wound outcomes
Learn to recognize and treat skin breakdown in dark skin.

By the year 2050, the non-Caucasian population of the United States will grow by 45%.1 How does that affect your practice? It’s more important than ever to understand how to properly assess, treat and prevent skin breakdown for people with dark skin tones.
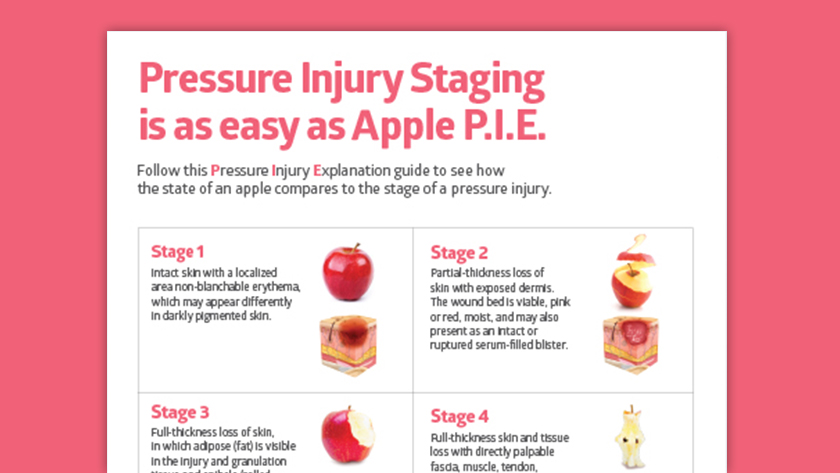
Unfortunately, nurse education often overlooks the differences between light and dark skin. Textbook materials and images have historically favored light skin,2 such as instructing nurses to look for “redness.”
People with dark skin are diagnosed with pressure injuries at later stages than people with light skin.3
Lack of experience with dark skin can lead to misunderstandings in practice and can negatively affect skin and wound outcomes.2 For example, people with dark skin are diagnosed with pressure injuries at later stages than people with light skin.3
It’s a situation that you can help turn around by following best practices when assessing and treating dark skin.
Skin color science
At the cellular level, all skin tones are essentially the same. There’s a misconception that non-Caucasian skin has more melanin, but scientific research shows that it’s actually the rate of melanin production and concentration of it that determines skin color.4 Dark skin produces melanin at a higher rate and it’s more concentrated than in light skin.
6 Tips to assess dark skin
Dark skin has certain qualities that call for unique assessment strategies. Here are six strategies to help assess dark skin.
1
Use your senses.
- Look for areas of skin that are darker than surrounding skin. Remember, dark skin rarely shows a blanching response. Instead, use a small pen light to better detect surrounding skin that’s taut, shiny or hardened. If you have access to advanced technology, visible and near-infrared spectroscopy have been shown to measure blanch response that isn’t dependent on skin color.5
- Feel for changes in skin temperature or tissue consistency, such as skin that’s waxy, firm or boggy.
- Smell a wound after it’s been cleaned to detect decaying or dead tissue.
- Listen to your patients. They may not know the medical terms, but if you ask them to describe what’s going on and actively listen to their answers, you’ll likely get valuable information.
2
Document in detail.
Be sure to take down patient history, as well as include plenty of description in your documentation. This practice helps provide a more personalized assessment instead of simply checking boxes. It’s interesting to note that research has indicated that clinicians of a different ethnic background than their patients tend to miss some tissue changes.4 To be as thorough as possible, consider pairing two caregivers to conduct the assessment together.

When dark skin is healing from a stage 3 or 4 pressure injury or other traumatic wound, it can sometimes take up to a year for natural pigmentation to return.4
3
Be aware of cultural customs.
During your assessment of someone with dark skin, you may encounter unfamiliar markings. Be sure to ask instead of assuming it’s skin damage. For example, some cosmetic, tribal or social customs may include cupping, spooning, acupuncture or body modifications that leave temporary or permanent marks on the skin.4
4
Prepare your patient for skin changes.
Although the cause is unknown, when dark skin is healing from a stage 3 or 4 pressure injury or other traumatic wound, it can sometimes take up to a year for natural pigmentation to return.4 This discoloration may be upsetting to a patient or their family, so it’s helpful to talk to your patient about the process. Also, remember that you may see areas of light skin that indicate a previous wound.
5
Take photos, but know their limits.
Digital photography is often not optimized to register dark skin as well as light skin, so colors can be inaccurate.2 When you photograph dark skin, be sure to also document with a color chart and descriptions.
6
Make some assumptions.
If a patient has just come out of a long surgery, it’s fair to assume that they may have a deep tissue injury at their sacrum, even if you don’t see a change. Intervene early with proper repositioning and offloading.
Considering skin and wound care products for dark skin
Many of your same everyday skin care products, including cleansers, protectants and barriers, may be effective on all skin types. But one thing to keep in mind with dark skin: Research shows dark skin may hold moisture differently than light skin,2 so it’s important to keep dark skin hydrated throughout the day. If you see dark skin looking ashy, it may be a sign to apply more moisturizer.
Research shows dark skin may hold moisture differently than light skin.2
When it comes to barriers, especially for incontinence, it can help to use a tinted product to better see how much you’re applying and how much remains after a certain time.
If you’re using dressings prophylactically or on damaged skin, a patient with dark skin may want a dressing to match their skin color. You can help explain that dressings aren’t intended to match anyone’s skin tone, but a light color, or even clear, can help provide visual cues that a dressing needs changing.
How to refer to skin color
In addition to important practices to ensure proper care for dark skin, it’s also important to use inclusive language when talking about dark skin. First, it helps to move away from thinking of dark skin as a “challenge,” and instead as one skin attribute among many.
Also, you may hear the phrase “darker skin tone,” but that implies it’s darker than other skin, which, in turn, implies that the “other” is the norm or the standard, and the dark skin is abnormal. “In wound care, it is important to remember that skin tone is separate from race,” state the authors of “Best Practice Statement: Addressing skin tone bias in wound care.”2
“In wound care, it is important to remember that skin tone is separate from race.”
Best Practice Statement: Addressing skin tone bias in wound care
When considering a neutral way to refer to skin color, it may be preferable to use “dark” or “non-white.” But how do you determine skin color? Here are a few common ways, and their pros and cons:

The Fitzpatrick Skin Type
Pro: Created in the 1970s, the simple Fitzpatrick scale is the most well known today.
Con: It wasn’t intended for skin assessment. It was created to help predict skin cancer risk through a patient’s own self-identification. Also, it has been found to be subjective2 and only offers six options, not accounting for a lot of variation.
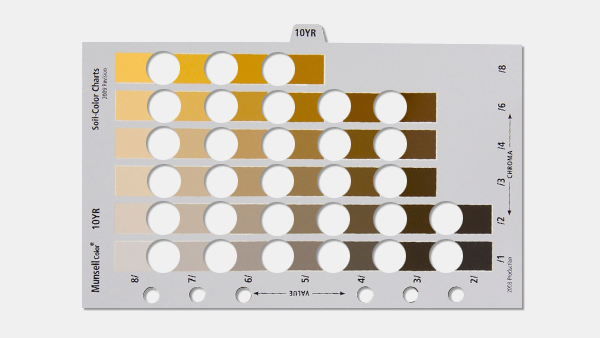
The Munsell color chart
Pro: Using a numerical system, Munsell includes more color shades than Fitzpatrick.
Con: It was meant to categorize items for agriculture and archaeology. The connotations of soil and dirt are not considered to be appropriate when determining skin tone.2
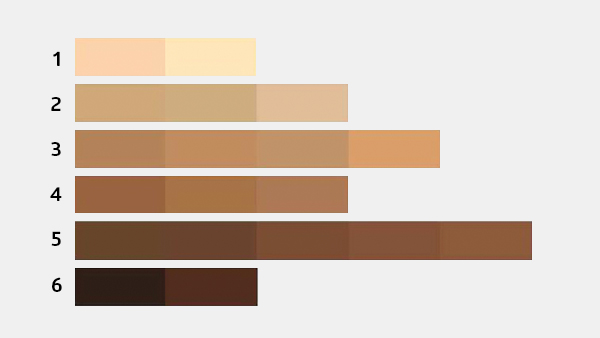
The color bar tool
Pro: This multi-hued bar chart has a broad range of skin color gradients and makes it easy for caregivers to identify skin tone by selecting the color that most closely matches a person’s inside upper arm.2
Con: May be more subjective
Key takeaway
In order to deliver exceptional care for all skin types, it’s important to know how to recognize, refer to and assess dark skin. The unique qualities of dark skin call for slight shifts in your skin assessment strategies, such as going beyond visual indications. Differences in skin color may also call for thoughtful interventions that help prevent and treat skin breakdown. Keep these top of mind to help make skin health second nature.
References:
- Passel, J. S., & Cohn, D. (2020, May 30). U.S. Population Projections: 2005-2050. Pew Research Center’s Hispanic Trends Project. https://www.pewresearch.org/hispanic/2008/02/11/us-population-projections-2005-2050/
- Wounds UK (2021) Best Practice Statement: Addressing skin tone bias in wound care: assessing signs and symptoms in people with dark skin tones. Wounds UK, London. Available to download from: www.wounds-uk.com
- Oozageer Gunowa, N. (2022). Wound management in people with dark skin tones. Nursing in Practice. https://www.nursinginpractice.com/clinical/wound-care/wound-management-in-people-with-dark-skin-tones/
- Public Health Live!, Hettrick, H., PT PhD CWS, CLT, CLWT, & School of Public Health, University at Albany. (2014, December 4). Skin & Wound Challenges in People of Color [Video]. https://vimeo.com/199889843
- Matas, A., Sowa, M. G., Taylor, V., Taylor, G., Schattka, B. J., & Mantsch, H. H. (2001). Eliminating the issue of skin color in assessment of the blanch response. Advances in skin & wound care, 14(4), 180–188. https://doi.org/10.1097/00129334-200107000-00010