Chronic wound treatment: 5 patient success stories
Discover faster healing with an advanced wound dressing.

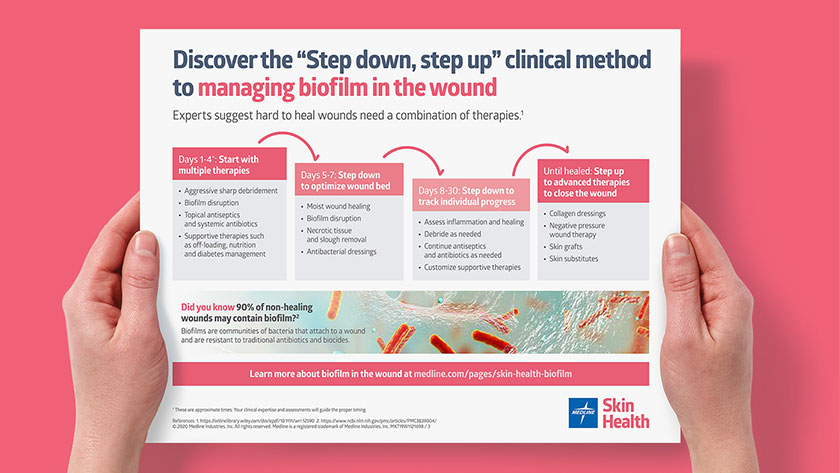
You strive to provide the best possible wound care, but patients with chronic wounds present complex challenges. Experts now agree that biofilm may be the cause of a stalled wound healing process. More than 90% of chronic wounds and some acute wounds may contain biofilm.1 Wounds such as venous leg ulcers, diabetic foot ulcers and pressure injuries may all contain biofilm.
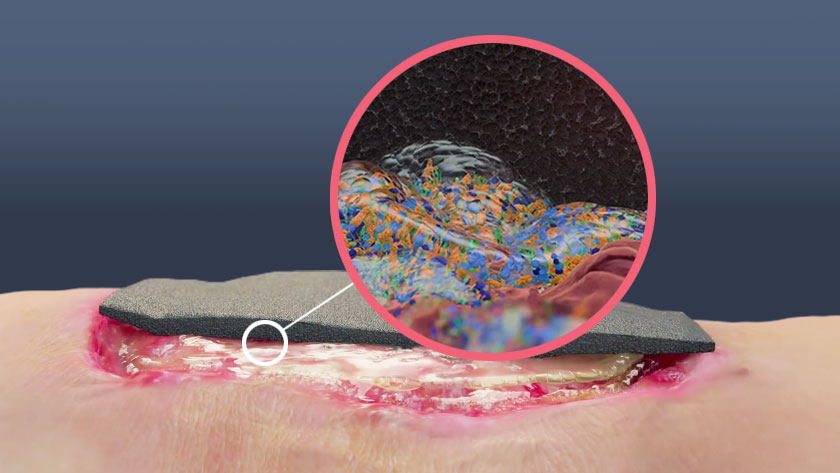
Biofilm in the wound
Biofilm is a community of bacteria that’s encased in a protective environment, making it more difficult for traditional therapies to work. That’s why it’s important to have the most advanced wound care products available to help promote wound healing.
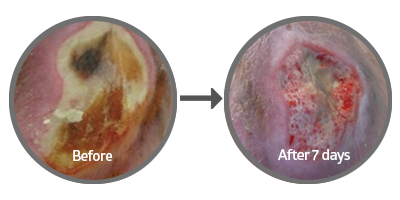
There are many choices for dressings for chronic wounds, but the innovative technology of PluroGel Burn and Wound Dressing uses surfactant micelles to hydrate the wound, control exudate and support autolytic debridement. It softens, loosens and traps debris to de-slough the wound bed, and helps remove necrotic tissue due to its surfactancy effect of the extracellular matrix. It has also been shown in vitro to both disrupt biofilm and prevent it from rebuilding based off in in vitro testing.2
The science behind PluroGel. Watch video
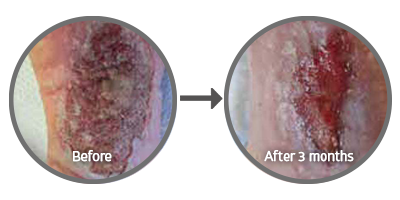
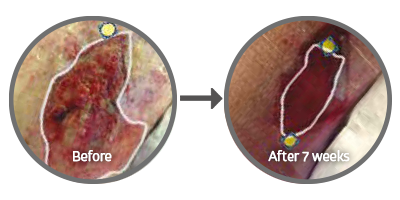
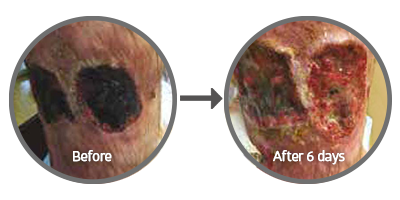
Below are five case studies that demonstrate the power of PluroGel as a therapy for managing chronic wounds in a timely manner.
Key takeaway
Biofilm may be a key factor in non-healing wounds, and it’s important to arm yourself with all the tools possible to kick-start the healing process. In many real-life cases of chronic wounds, PluroGel Burn and Wound Dressing has been shown to make a significant impact on helping these wounds to shrink and become less painful.
References:
- Attinger C and Wolcott R. Clinically addressing biofilm in chronic wounds. Advances in Wound Care. 2012;1(3):127-132. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3839004/. Accessed September 16, 2019.
- Yang Q, Larose C, Porta AD, Della Porta AC, Schultz GS, Gibson DJ. A surfactant-based wound dressing can reduce bacterial biofilms in a porcine skin explant model. Int Wound J. 2016
- https://doi.org/10.12968/jowc.2018.27.10.664, courtesy Rosemary Hill BSN, CWOCN, WOCC (C), VCH-Coastal-Lions Gate Hospital
- https://doi.org/10.12968/jowc.2018.27.10.664, courtesy Dot Weir, RN, CWON, CWS, Clinical Staff, Saratoga Hospital Center for Wound Healing and Hyperbaric Medicine, Saratoga Springs, NY
- Hill, R., BSN CWOCN CETN(C) & Vancouver Coastal Health-Lions Gate Hospital. (n.d.). Need a biofilm disrupter? Consider application of a concentrated surfactant technology: A case series.
- Ratliff, C. R. (2018). Management of a Groin Wound Using a Concentrated Surfactant-Based Gel Dressing. Journal of Wound Ostomy and Continence Nursing. https://doi.org/10.1097/won.0000000000000467