The clear wound dressing that’s the future of PI prevention
Discover OptiView® Transparent Dressing with HydroCore™ Technology.

Caregivers know well that foam dressings are effective for preventing and treating pressure injuries (PIs). But when it comes to skin checks, it’s often a challenge to remove the dressing multiple times per day.
This process eats up time for caregivers who are stretched thin, and it puts stress on the dressing’s adhesive and fragile underlying skin.
“We have to assess the skin under the dressing every shift. In order to do that, the nurses need to remove the dressing,” says Layla Nejati, WOCN at Danbury Hospital in Connecticut. “We had to change the dressing daily, which had a huge financial effect for us.”
Wouldn’t it save time and cut waste if there was a transparent wound dressing that caregivers could use as part of their PI prevention protocol? One that gave them constant visibility of at-risk skin without sacrificing protection against pressure and shear?
Now, there is.
The future of PI prevention is clear
Nurses were recently introduced to a first-of-its-kind clear prevention dressing through a poster presentation at the latest NPIAP conference in March.
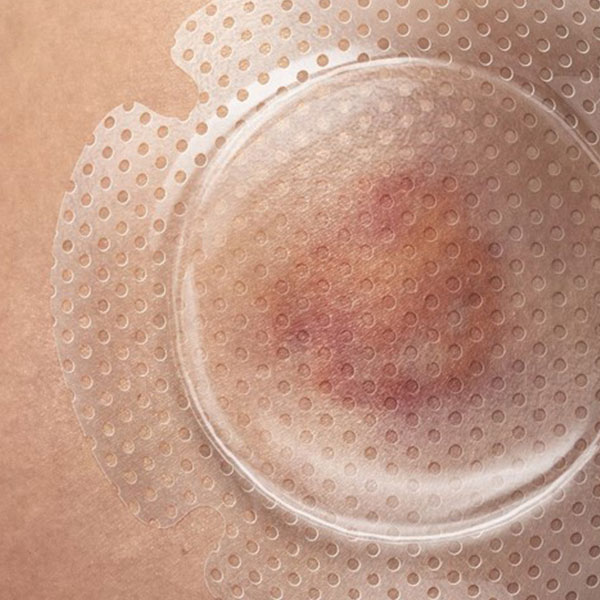
OptiView® Transparent Dressing with HydroCore™ Technology is a gamechanger for PI prevention. The transparent prevention dressing has a clear island that effectively eliminates the lift-and-check approach of traditional prophylactic dressings.
While there’s still a place for foam in their protocols, caregivers are excited to add OptiView to their list of proven interventions for shielding intact skin from breakdown.
Doing more with less: Connecticut hospital improves outcomes with clear wound dressing

Nejati had the opportunity to pilot OptiView in the ICU on 20 patients at Danbury Hospital. With this transparent wound dressing, her team no longer had to do daily dressing changes. They were able to extend the wear time up to 5 days in some cases. This had a significant impact and improved clinical and financial outcomes. As a result, Danbury was able to do more with less.
6 reasons why the caregivers at Danbury Hospital raved about OptiView:
- Ability to assess skin without removing the dressing
- Sacral dressing wear time of 3-5 days, sometimes longer
- Dressing wear time on hips and shoulders of 4-5 days
- Drop from 300 to 100 sacral dressings used per month
- Substantial cost and time savings
- Reduced risk of medical adhesive-related skin injury (MARSI)
- High nurse and patient satisfaction
Clear visibility saves time and reduces waste
One feature that makes OptiView so unique is its clear island. It allows caregivers to do a skin assessment without lifting the dressing. They can inspect, monitor and blanch through the clear island and spot everything from skin texture to color variances to early signs of breakdown.
For Nejati, that was the biggest benefit of OptiView. “As a wound nurse, you always want to look to see what’s going on underneath a dressing.”
“Financially it had a huge effect, and it saved nurses a lot of time.”

Layla Nejati
WOCN at Danbury Hospital in Connecticut
For Nejati and her team, this led to other positive outcomes. She adds, “Financially it had a huge effect, and it saved nurses a lot of time.”
She estimates that dressing changes can eat up anywhere from three to 15 minutes of staff time. With so many facilities facing limited staffing resources, the time saved quickly adds up and creates more time for direct patient care.
Helps keep skin up to 1.5° C cooler than leading foam dressings
Caregivers know that managing the microclimate—the interaction between skin temperature and moisture at its surface—is key to PI prevention. OptiView helps keep skin cool and lock out moisture.
That’s important—every 1° C increase in temperature results in a 10% increase in metabolic demand, putting skin at risk for breakdown.1
OptiView is shown to release heat better than leading foam competitors. The thermal images below show that this clear wound dressing keeps skin up 1.5° C cooler than these foam dressings.2
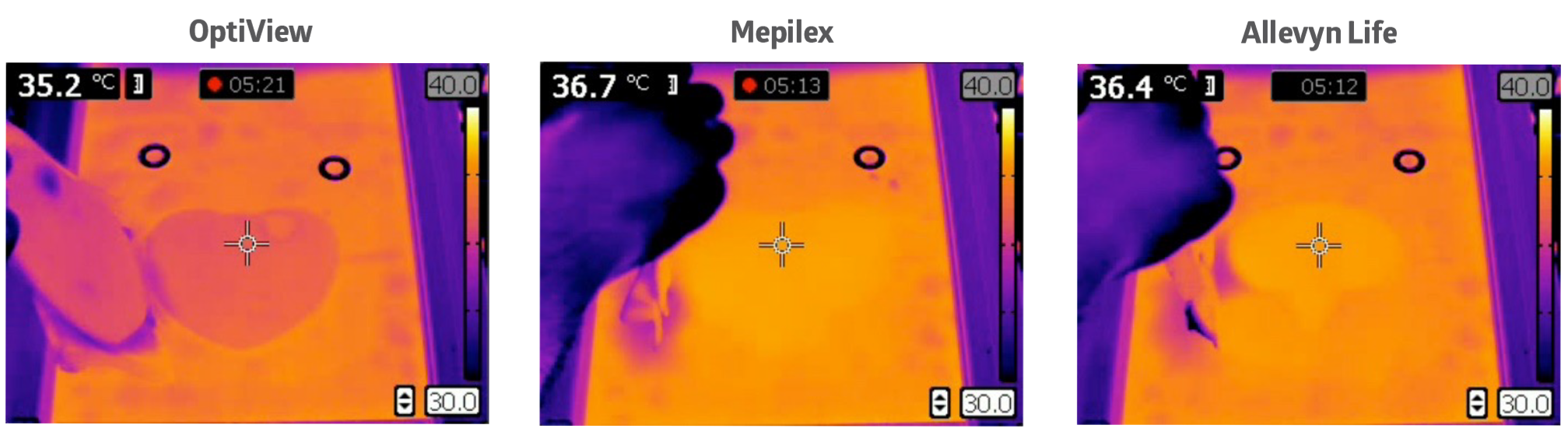
How does OptiView achieve this? Its HydroCore technology uses a gel to pull heat away from the skin. It creates a cooling effect just like the gels in therapeutic mattresses and other support surfaces designed to help prevent PIs. Additionally, the transparent wound dressing features a waterproof backing to protect the underlying skin from moisture.
By managing the skin’s microclimate, it reduces the risk for pressure injuries.
For the more alert patients in her ICU, Nejati was able to ask them about how the dressing felt on their skin. When asked about the cooling effect, she said, “All of my patients loved it.”
Reduces peak pressure and shear
For preventing PIs on intact skin, OptiView functions like a foam dressing and allows caregivers to follow the best practice guidelines of the NPIAP and international organizations for an appropriate prophylactic dressing.3
HydroCore technology, in addition to managing microclimate, also helps with reducing peak pressure and shear—all contributing factors that cause PIs. Like a therapeutic mattress or other support surfaces designed to help prevent PIs.
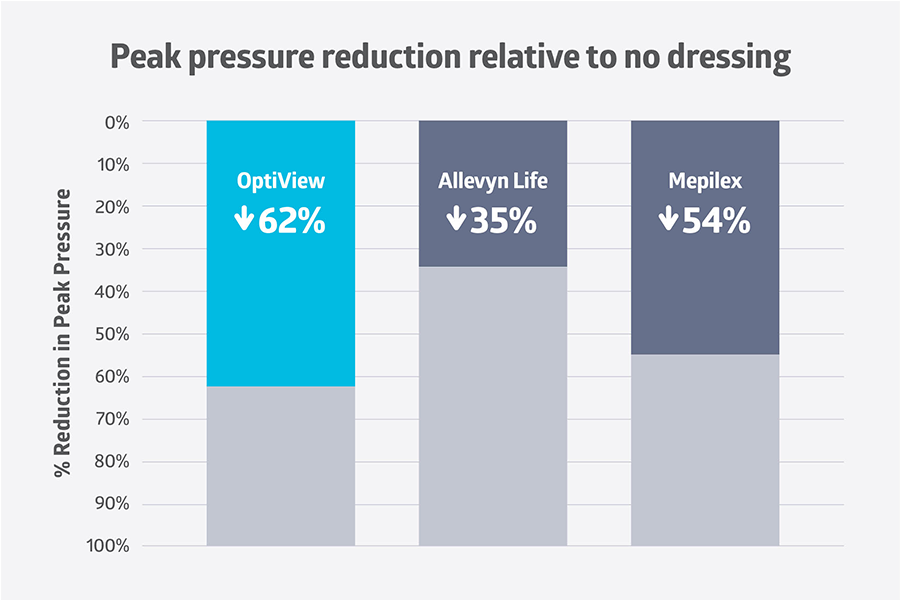
For intact skin, OptiView reduces shear as well as five-layer foam dressings, and it had the highest peak pressure reduction—by as much as 62%—among market leading dressings.4
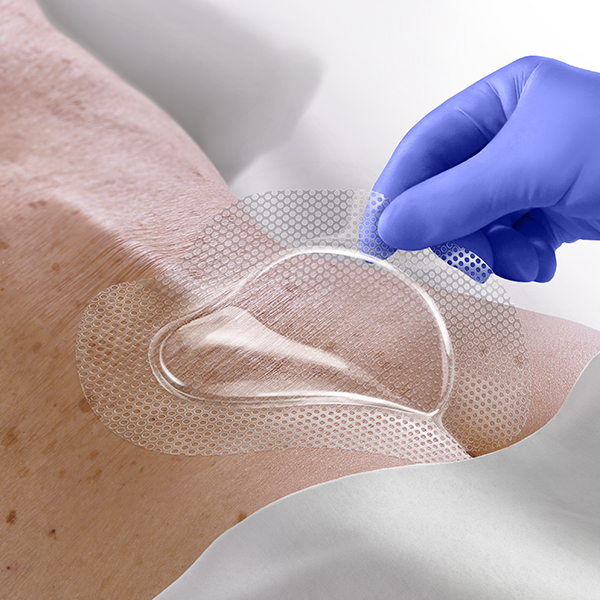
It’s designed to work on the bony prominences most at risk for PIs. With a dressing shaped especially for the sacrum and a round multi-site shape, it fits perfectly over the most vulnerable areas.
Improves patient comfort
In addition to the cooling effect that Nejati’s patients enjoyed, the transparent wound dressing has other features to aid with patient comfort.
Greater dressing flexibility—up to 12 times more flexible than leading multilayer foams—allows OptiView to adapt to patient movement.5 The result is that the patient can wear the dressing longer without it being changed, resulting in less stress on the underlying skin.
Some nurses use the dressing under neck collars and other devices to protect skin against medical device-related pressure injuries (MDRPIs).
It also has a silicone face and border to aid in gentle removal.

Key takeaway
OptiView simplifies skin assessments while performing as well as traditional foam dressings against the forces that cause PIs, and it outperforms these dressing when it comes to releasing heat. Nurses are adding it to their list of proven interventions for PI prevention and are using it alongside foam to protect intact skin. Studies confirm OptView benefits for patient care, and a clinical trial showed that it leads to fewer dressing changes, resulting in significant cost and time savings.
References:
- Brown AC, Brengelmann G. Ch. Energy metabolism. In: Ruch RC, Patton HD, editors. Physiology and biophysics. 19th ed. Philadelphia, PA: WB Sanders; 1965. Chapter 53, pp. 1030-49.
- Data on file.
- European Pressure Ulcer Advisory Panel, National Pressure Injury Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline. The International Guideline. Emily Haesler (Ed). EPUAP/NPIAP/PPPIA: 2019.
- Data on file.
- Data on file.
