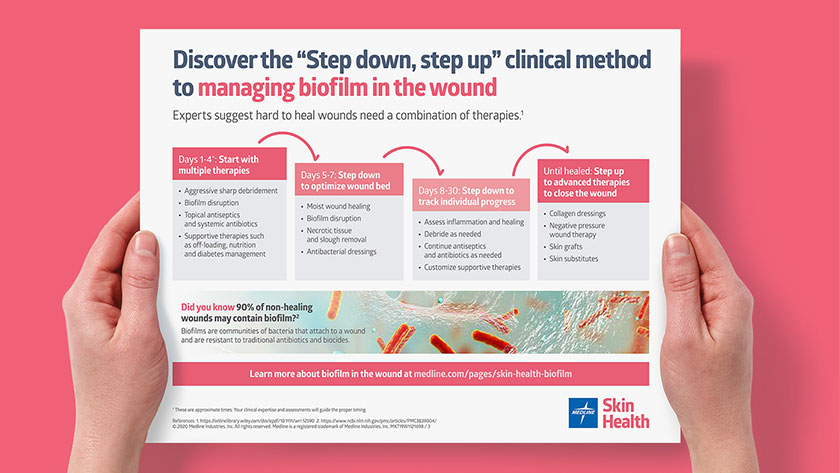
Bacterial biofilm: What it is and how to reduce its impact on wound healing
Get the latest tools to manage biofilm and help improve wound outcomes.
You know that fuzzy film you sometimes feel on your teeth first thing in the morning? That’s biofilm. Dentists refer to it as plaque and have long understood its negative effects on the health of your teeth. They encourage daily brushing and flossing to effectively manage bacterial biofilm growth.1
Biofilm has only been a buzzword in wound care for the past two decades or so, but it has taken on vital importance in the war against chronic wounds.2
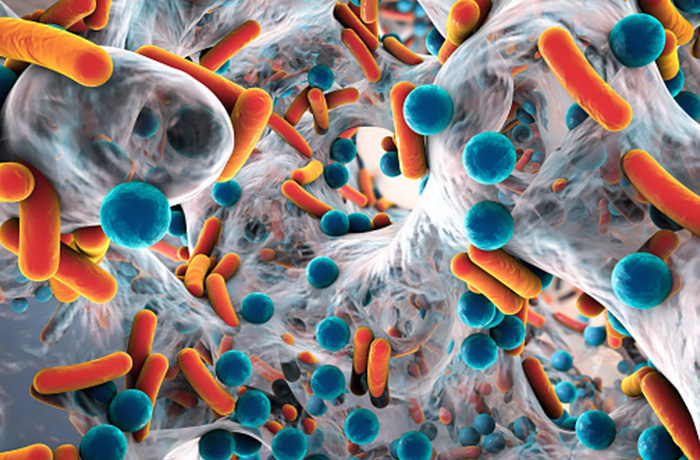
What is biofilm? Biofilms are communities of bacteria that are covered in a polysaccharide matrix. This unique biofilm structure translates to a slimy barrier of sugars and proteins. Almost all hard-to-heal wounds have some amount of biofilm.3, 4
90%
of non-healing wounds may contain biofilm 5
How biofilm infections affect wound care
The frustrating part for your work on wounds is that biofilm structures are notoriously tolerant to antibiotics and seemingly protected from the patient’s natural immunities, which contributes to the wound’s chronic character.
In fact, studies show that biofilm bacteria can be up to a 1,000 times more resistant to antibiotics than free-floating bacteria of the same species.6
“We are just now seeing more and more research into how microbial biofilms can affect a body’s ability to heal wounds and what treatments can most effectively create an optimal wound healing environment,” says Medline Clinical Education Specialist Katie James BA, RN, CWCN.
Understanding the formation of biofilms
There are three stages to biofilm formation:3, 7, 8
1. Attachment to the surface: First, planktonic, or free-floating, bacteria attach themselves to the wound.
2. Colonization: Given the time and opportunity, bacteria band together into a diverse community that changes to promote its own survival.
3. Critical colonization: This is the mature state of biofilm when it secretes its slimy covering known as the extracellular polymeric substance (EPS), serving as powerful protection against the patient’s immune system and traditional antimicrobials.
Following that last step, a fourth step often occurs when free-floating bacterial species may then detach from the structure to form new colonies. When that happens, the person’s immune system responds again, creating a “chronic relapsing infection.”6
Learn more about the science behind biofilm formation and biofilms in chronic wounds.
Watch the video
When to suspect biofilm forming in wounds
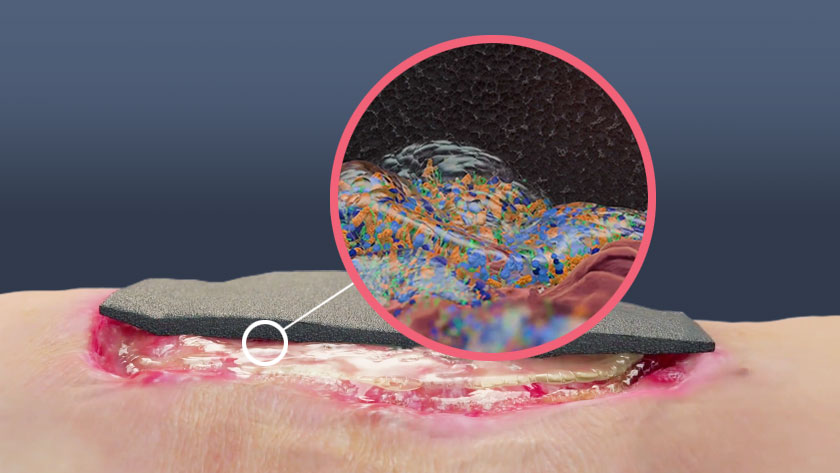
Biofilm is sneaky because routine lab tests can’t differentiate between floating bacteria and attached bacteria. Plus, biofilms growing under the surface of the wound make it even more challenging to know what’s really going on.9
“Trying to see biofilm with your naked eyes is like trying to see the wind. In reality, we only see the result of the wind.”

John P. Kennedy
RPh, PhD, research professor, South University School of Pharmacy, and Medline consultant
The unique structure and EPS barrier of biofilm kills tissue in a slow, steady process that, if gone unchecked, can have devastating consequences. “The end result is typically some type of surgical removal of degraded tissues,” explains Dr. Kennedy. “In wound care, too often, that could mean amputation.” Before biofilm gets the upper hand, look out for qualities in the wound that might signal its existence.
The International Wound Infection Institute’s Consensus Update 2022 on Wound Infection in Clinical Practice outlines some criteria that can help you identify potential biofilm formation on your patients’ wounds:4
- Failure of appropriate antibiotic treatment
- Resistance to appropriate antimicrobial treatment
- Recurrence of delayed healing after antibiotic treatment
- Delayed healing despite optimal wound management and health support
- Increased exudate or moisture
- Low-level chronic inflammation
- Low-level erythema
- Poor granulation or friable/hypergranulation
- Secondary signs of infection
- Myth: You can see biofilm
Truth: Biofilm is microscopic and, although it might cause a wound to have certain characteristics, the biofilm itself cannot be readily detected. “Trying to see biofilm with your naked eyes is like trying to see the wind,” says John P. Kennedy RPh, PhD, research professor, South University School of Pharmacy, and Medline consultant. “In reality, we only see the result of the wind.” - Myth: A wound swab can identify biofilm
Truth: In fact, wound swabs are only effective at identifying planktonic bacteria, not biofilm. So this is not a method to rely on. - Myth: Antibiotics or a topical antimicrobial will get rid of biofilm
Truth: Unfortunately, antibiotics alone won’t successfully treat biofilm because they can’t get through the strong extracellular matrix that covers the community of bacteria in the wound. Before any antibiotics will work effectively, aggressive and sustained measures to break down biofilm and prevent its regeneration must be accomplished first. - Myth: Honey is an effective treatment
Truth: Although Manuka honey has been used for hundreds of years as an agent in wound healing, in the case of biofilm, it has now been shown that honey actually might do the opposite and make persister bacteria in the biofilm more immune to honey’s mechanism of action. - Myth: It’s the dressing that isn’t working
Truth: Caregivers may be tempted to blame a dressing for a wound not progressing, but it may be the wound environment of biofilm that is a barrier to healing. Sometimes it’s not what you put on a wound but what you take off it that allows it to heal. - Myth: Dakin’s solution beats biofilm
Truth: This bleach with water and buffer solution might disrupt biofilm for a short time, but the solution is cytotoxic and therefore damages healthy tissue which can delay wound healing. Beating biofilm requires a more balanced approach to penetrate the extracellular polymeric matrix and preserve healthy tissue. - Myth: Wet to dry dressing changes are effective
Truth: Wet to dry healing is no longer recommended because it’s been shown to strip away granulation tissue, which disrupts healing. Maintaining a moist wound bed is the recommended method now. Also, wet to dry healing can be painful, can promote wound bed trauma and doesn’t penetrate deeply rooted biofilm under the surface. - Myth: Sharp debridement gets rid of biofilm
Truth: Sharp debridement is often used to manually remove debris, slough and necrotic tissue, but it doesn’t fully eliminate biofilm and it doesn’t prevent biofilm from re-establishing itself. As a result, biofilm left in the wound can overwhelm the host, and the wound may remain stalled. Sharp debridement can be used as part of a holistic strategy to fight biofilm. However, it’s important to note that sharp debridement may be contraindicated in certain patients and require topical agents with proven anti-biofilm properties.
Manage biofilm with the right system of products
Standardizing a treatment protocol may help manage biofilm on a wound to help wound healing. “Since biofilm is found in such a high population of chronic wounds, it has to be a part of any discussion regarding wound healing and treatment practices today,” James says.
In addition to the negative effects for the patient, James notes, “The longer it takes to heal a wound, the increased cost to heal that wound.” The right treatment can speed your patient’s healing time and reduce expenses for your patients and the healthcare facility.
Treating biofilm can be situational. The three tactics below are not a linear timetable, but rather offer an interactive approach.
3 strategies for the effective management of biofilm
When it comes to choosing products, there are several important goals to consider.4, 9, 10
Debride the wound – It’s essential to include debridement in your biofilm management in order to help disrupt biofilm in the wound and promote wound healing. Debridement options include sharp debridement, autolytic, mechanical, enzymatic and surfactant.


How an iodine dressing can control biofilm and reduce bacteria
Iodine has been used in wound care since the American Civil War. Scientists believe that its value is related to its ability to penetrate the cell wall of micro-organisms.11 While silver has been a standard in hard-to-heal wound care, numerous in-vitro studies show that iodine is better at controlling biofilm than other antibacterial agents.12
“With the ability to have a controlled release platform, IoPlex has become an effective agent in managing the biofilm activity.”

Katie James
BA, RN, CWCN, Medline Clinical Education Specialist
“There are only a few true antibacterials on the market, and silver has been the number one go-to, even though iodine actually has a broader spectrum of effectiveness than silver,” James explains. “The problem with iodine is that, alone, it is also cytotoxic, meaning that it kills the good with the bad. Now, with the ability to have a controlled release platform, IoPlex has become an effective agent in managing the biofilm activity.”
Developing protocols and using effective tools will help your team manage biofilm in wounds.
Key takeway
Biofilm may be to blame for hard-to-heal wounds—and one of the reasons why your job is so important. Although treating biofilm is challenging because of its tolerance to typical antibiotics, if you know the signs to look for and the right products to use, you can help improve healing outcomes for your patients. Product innovations to manage biofilm, such as the effective use of a concentrated surfactant and iodine, could be your secret weapon.
References (All accessed May 13, 2020):
-
Saini, R., Saini, S., & Sharma, S. (2011). Biofilm: A dental microbial infection. Journal of Natural Science, Biology, and Medicine, 2(1), 71. https://doi.org/10.4103/0976-9668.82317
-
MSU wins millions to find treatments for slow-healing wounds. (n.d.). Montana State University. https://www.montana.edu/news/3874
-
Bjarnsholt T, Eberlein T, Malone M, Schultz G. Management of wound biofilm Made Easy. London: Wounds International 2017; 8(2).
Available from: www.woundsinternational.com -
International Wound Infection Institute (IWII) Wound infection in clinical practice. Wounds International 2016
-
Attinger, C., & Wolcott, R. (2012). Clinically Addressing Biofilm in Chronic Wounds. Advances in wound care, 1(3), 127–132. https://doi.org/10.1089/wound.2011.0333
-
Biofilm bacteria (MPKB). (n.d.). https://mpkb.org/home/pathogenesis/microbiota/biofilm#life_cycle_of_biofilm_communities
-
Wu, Y., Cheng, N., & Cheng, C. (2019). Biofilms in Chronic Wounds: Pathogenesis and Diagnosis. Trends in Biotechnology, 37(5), 505–517. https://doi.org/10.1016/j.tibtech.2018.10.011
-
Cwcms, K. S. M. (2021, July 27). Wound Detective Series: How to Get Away with Killing Biofilm |. WCEI.
https://blog.wcei.net/wound-detective-series-how-to-get-away-with-killing-biofilm -
Schultz, G. S., Bjarnsholt, T., James, G. A., Leaper, D., McBain, A. J., Malone, M., Stoodley, P., Swanson, T., Tachi, M., & Wolcott, R. D. (2017). Consensus guidelines for the identification and treatment of biofilms in chronic nonhealing wounds. Wound Repair and Regeneration, 25(5), 744–757. https://doi.org/10.1111/wrr.12590
-
Yang Q, Larose C, Della Porta AC, Schultz GS, Gibson DJ. A surfactant-based wound dressing can reduce bacterial biofilms in a porcine skin explant model. Int Wound J. 2017 Apr;14(2):408-413. doi: 10.1111/iwj.12619. Epub 2016 May 22. PMID: 27212453; PMCID: PMC7950006.
-
Sibbald RG, Leaoer DJ, Queen D. Iodine Made Easy. Wounds International 2011; 2(2): Available from http://www.woundsinternational.com