CABSI prevention: Every catheter port needs a cap
5 proven ways to help reduce CABSIs using disinfection caps.
Clinicians work hard to keep up with guideline changes, new protocols and new products. But it’s not always easy. Healthcare environments move fast and sometimes new products and techniques are introduced without enough explanation or training.
In the webinar Every Port Needs a Cap, Jill Nolte, BS, BSN, Medline Clinical Resource Manager, provides the detail clinicians want and need around INS guidelines and disinfection cap use to prevent catheter-associated bloodstream infections or CABSIs.
Every Port Needs a Cap: How to use disinfection caps to reduce CABSIs
Infusion clinicians know the challenge of preventing catheter-associated bloodstream infections (CABSIs). Insertion bundles have helped, but care and maintenance of venous catheters are receiving renewed attention. Leading vascular access management expert Jill Nolte explains new 2021 Infusion Nurses Society (INS) guidelines around catheter hub disinfection and the prevention of intraluminal contamination that can cause CABSIs. Using an engaging combination of Q&A, polling and presentation, Nolte addresses the disinfection of needleless connectors, disinfection cap use and how you can help your facility achieve zero harm.

Nolte remembers her own confusing introduction to disinfectant caps as a cardiac floor nurse. The caps just “showed up” without an in-service or any training, she recalls, and her team was simply told to put them on patients’ lines.
“This is how so many things come to nurses in fast-moving hospital environments—without enough explanation of the ‘why’,” says Nolte, who later managed a hospital vascular access program. “We wondered at the time, should they go on all lines or just central lines? Can you reuse them? Why use them? One package said a cap was good for seven days, but it didn’t say—only if not removed. So some of us were reusing caps thinking we were following protocol perfectly.”
Nolte knows that even though it’s hard to find time, training to build understanding and compliance pays off in reduced infection rates. Her engaging webinar presents everything clinicians need to know about needleless connectors, INS recommendations and disinfection cap use.
Here are five key webinar highlights:
1 | Use disinfection caps the right way and reduce CABSI
Nolte explains how needleless connectors solved the needlestick and disconnection problems of earlier catheters but bring with them an increase in CABSIs. Caps offer the solution to that problem—“technique-free” disinfection that is proven to reduce CABSI.
Recommended by the INS, caps overcome inconsistencies in “scrub the hub” disinfection techniques. They’re more effective than alcohol wipes alone and provide a physical barrier against environmental and other contaminants for up to seven days if not removed.
2 | Cap all lines, not just central lines
As Nolte says, there’s always been a focus on infection originating in central lines, but awareness is growing that peripheral IVs cause infection, too. Pathogens can enter from any catheter access point, so capping all of them is considered best practice by INS and many other global quality organizations including SHEA and ECRI.
3 | Make ANTT (Aseptic non-touch technique) easy
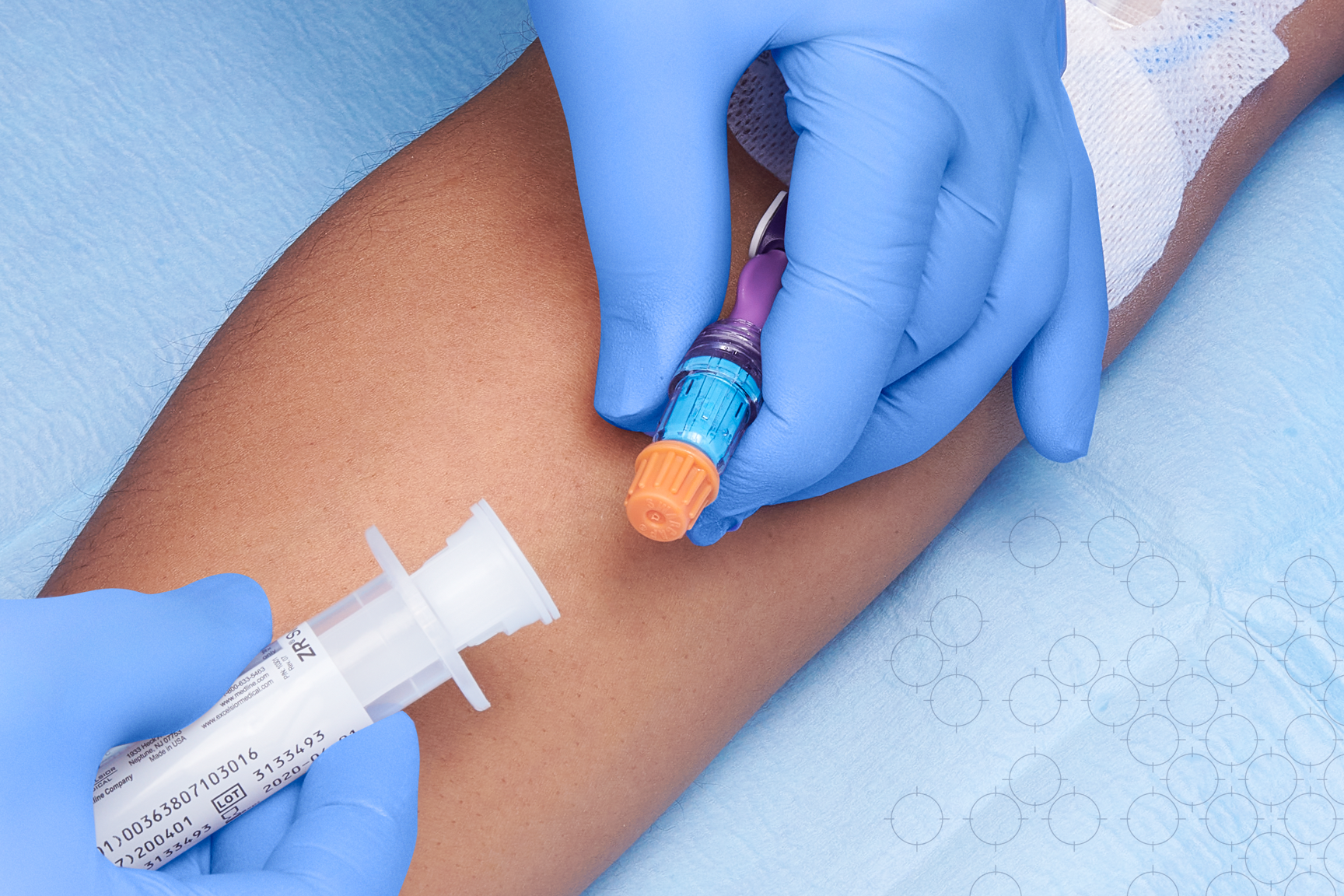
When flushing lines, it’s sometimes hard for clinicians to hold everything in their hands. Supplies can be mistakenly set on non-sterile surfaces. Providing caps to clinicians in a way that makes it easy to comply with ANTT helps. Using a flush syringe with an integrated disinfection cap supports aseptic practice and helps to improve compliance as the cap is right there when needed. Using dressing change systems that support aseptic technique is also important.
4 | Choose a cap with care
Nolte explains that cap disinfection times can vary from 30 to 60 seconds as the connector hub and threads bathe in 70% alcohol. Some caps offer continuous disinfection for seven days if not removed. And a non-vented cap provides an impermeable barrier to airborne, touch and fluid contamination.
5 | Educate, monitor and reward proper cap use across units
CABSI rates decrease when staff are trained and leaders establish clear policies. Nolte describes how successful efforts must include everyone—leaders, infection preventionists, vascular access teams throughout the facility and anyone who inserts and removes IVs, including homebound patients.
To help keep best practices top of mind, Nolte recommends in-services and reminder posters, conducting frequent compliance assessment audits, rewarding staff and units for consistent capping and keeping staff updated on their performance and infection reduction trends.
Looking for more ways to help your clinicians keep patients safe from CABSIs?
Create a culture of CABSI prevention with this proven Vascular Access Health Solution.
Watch best practice videos on vascular access infection prevention and CVC insertion bundles.
Improve catheter care with insights from the BSI 2019 Discovery Assessment Findings.
Sign up for a BSI Discovery Assessment to identify gaps in care at your facility and receive a customized action plan to help improve infection rates.
