Medical device design: Its role in best practices in healthcare
Learn how all-inclusive kits contribute to CAUTI and CLABSI prevention.

Why are smart devices intuitive to use—even for young children? Because the product designers have constantly observed human behavior, refined their products based on how consumers have used them in practice and ultimately created a culture where users intuitively understand how to use a new, somewhat familiar device.
These innovative designers have been able to anticipate user behavior and make it difficult to do the wrong thing. If the healthcare industry could adopt this human factors mindset, it would have the ability to develop medical products designed so that the right way is the only way to use the product.
Intuitively designed medical products have the potential for immeasurable positive impact on patient outcomes, costs and satisfaction among both patients and caregivers. That’s obviously easier said than done. Manufacturers have to understand clinician behavior well enough to ensure that a majority of nurses, physicians and other staff would use the product in a single way that leads to the best outcomes.
In other words, use and function should be obvious. But how?
Using an integrated approach
Clinicians, engineers, designers and manufacturers should be working together to create holistic solutions. Intuitively designed products take into consideration the normal context and behavior in which a device is used in the clinical setting. To understand what’s intuitive to physicians, manufacturers should carefully observe how clinicians use a product, including how they understand risk or harm and how they view convenience and efficiency.
Clinician behavior also can vary from a busy emergency department to a more relaxed doctors’ office, so it’s crucial to observe use in a variety of contexts. Although it can come at a higher cost, that cost is justified—healthcare manufacturers need to become better social scientists and take a more human-study approach for the sake of patient safety.
Medline designs its products with clinical intuition in mind. Some are even designed by frontline clinicians to overcome daily challenges. Let’s take a look at a few examples.
The Challenge
Variation and error can occur when clinicians perform even the simplest procedures with different products or using different techniques.
The Solution
All-encompassing kits with standardized products organized in order of use that guide clinicians and prevent variation. Designed by clinicians for clinicians, Medline’s kits make it easy for staff to perform a consistent procedure following evidence-based best practices.
Nurses change sterile dressings and access central venous catheter (CVC) lines numerous times a day with numerous patients. And inserting a central line is an invasive, complex process. The insertion and maintenance of urinary catheters is also a common occurrence. While clinicians may perform these procedures repeatedly, it doesn’t mean they do it the same way every time, and it certainly doesn’t mean every clinician does it the same. Outcomes—most importantly, infection rates—can vary widely based on the products used, the techniques employed and the precautions taken.
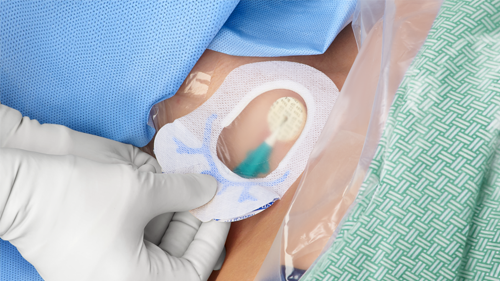
Based on clinical guidelines, Medline’s Vascular Access Health Solution and Urological Solution steer clinicians toward standardization via intuitively designed packaging and component sequencing that take them step-by-step through procedures. The Total One Layer IUC Tray helps prevent catheter-associated urinary tract infections (CAUTIs), while the ERASE BSI Customizable Dressing Change Kit and CVC Insertion Kit help limit central line-associated bloodstream infections (CLABSIs).
Total One Layer IUC Tray
Patients can be at risk for infection when clinicians use different products and techniques for insertion, securement, perineal care and timely removal of indwelling urinary catheters (IUCs).
“Traditionally, manufacturers have manufactured products but not spent as much time thinking about how to make it easier for clinicians to do their jobs,” says Donna Matocha, Medline’s Manager of Clinical Resources – Critical Care. “This changes the scope of things and says, ‘not only are we going to make a product, but we’re going to make a product that nurses want to use and is safer for patients.’”
Medline’s Total One Layer IUC Tray:
- Helps clinicians determine when to use a Foley catheter by including a list of clinical criteria on the tray label
- Promotes aseptic technique by including all necessary components sequenced left to right in order of use, securement and bacterial protection
- Contains standardized clinician instructions with clear illustrations
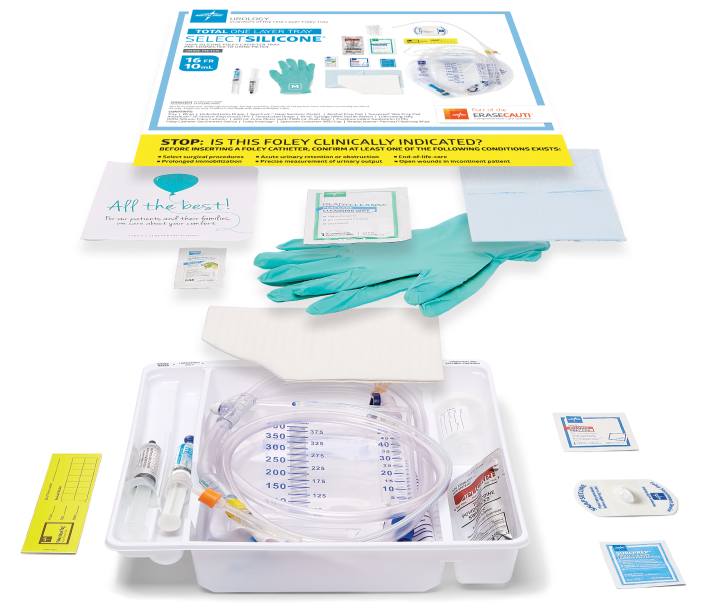
But the Total One Layer IUC Tray is built with an interesting difference: If clinicians are correctly following instructions, use of the kit may be limited. In its efforts to carefully standardize the procedure for catheterization, the Total One Layer IUC Tray is actually designed to warn clinicians against catheterizing unless it’s absolutely necessary.
It may seem counterintuitive for a manufacturer to steer clinicians away from using their product, but prolonged Foley use can lead to CAUTIs, which can lead to sepsis, a major contributor to hospital deaths.
Based on the fact that 2.5 million Foley catheters are placed without an appropriate indication each year, Medline put the best interest of patients first and made it easy for clinicians to do the same, Matocha says. So, a tab on the front of the Total One Layer IUC Tray alerts clinicians to “STOP” and question whether there’s a valid clinical reason for inserting a catheter, whether it be prolonged immobilization, end-of-life care, acute urinary obstruction or another listed condition.
The Total One Layer IUC Tray was created with significant input from frontline clinicians. Trent Haywood, MD, former Chief Medical Officer at the Blue Cross Blue Shield Association and an expert in human factors, led a team of researchers who observed use of the Total One Layer IUC Tray and helped refine it to ensure clinicians were using it effectively and as intended.
For example, the team found that the traditional two-layer tray created opportunity to perform the procedure in different ways, while the one-layer tray contained all the items needed and sequenced left to right so that caregivers performed the procedure the same way every time. The innovative one layer tray reduced variation in practice and promoted aseptic technique.
Lapses in practice can happen in a busy healthcare facility with limited staff, impacting patient care and safety. In healthcare settings, human failure can cause up to 90% of such errors.1
ERASE BSI Customizable Dressing Change Kit
CLABSIs can occur during CVC insertion, access or maintenance. As the Centers for Disease Control and Prevention (CDC) and other regulatory organizations have improved their guidelines for the prevention of CLABSI, the rate of CLABSIs that occur during insertion has decreased, leaving the remainder of infections to be caused by variation in central line maintenance.
Accessing the line happens multiple times a day—each time creates the potential for infection and cross contamination. In addition, friction and fluids can damage the skin at the insertion site, creating a path to infection.
Seeking to create a product that would help reduce the rate of CLABSIs, Medline product managers gathered a collection of products that could assist in the fulfillment of CDC recommendations. But all of these products were readily available to any clinician, so what’s the real problem? Why aren’t all caregivers changing sterile dressings in the same way?
“We discovered it was really in the way those products are given to clinicians to use,” said Angela Newman, Medline’s Senior Director of Clinical Services – Acute Care.
Traditional dressing change kits typically have come in a peel-back pouch, packed in no particular order and rarely containing everything a clinician needs to perform a sterile dressing change. As a result, clinicians often needed to find other products to supplement the pack, depending on what kind of line dressing they were changing, or how they were accessing. This deviation from the pack—an opportunity for clinician preference—is a key point at which variation can take place.
“It gave us a clear indication that if everything doesn’t come with the kit, people aren’t doing it the same way every time,” Newman says. “We realized if we could design a kit in a way that could take them through the process step-by-step in a standardized manner, they’d be less likely to forget a step, make an error or deviate from best practice.
Designed by nurses for nurses, Medline’s ERASE BSI Customizable Dressing Change Kit:
- Makes it easier for clinicians to perform a consistent procedure no matter how busy or inexperienced they are
- Includes all products, organized in a left-to-right sequence to ensure the right product is used at the right time
- Creates a sterile work area and organizes all components to prevent contamination at every step
- Includes numbered instructions with clear illustrations
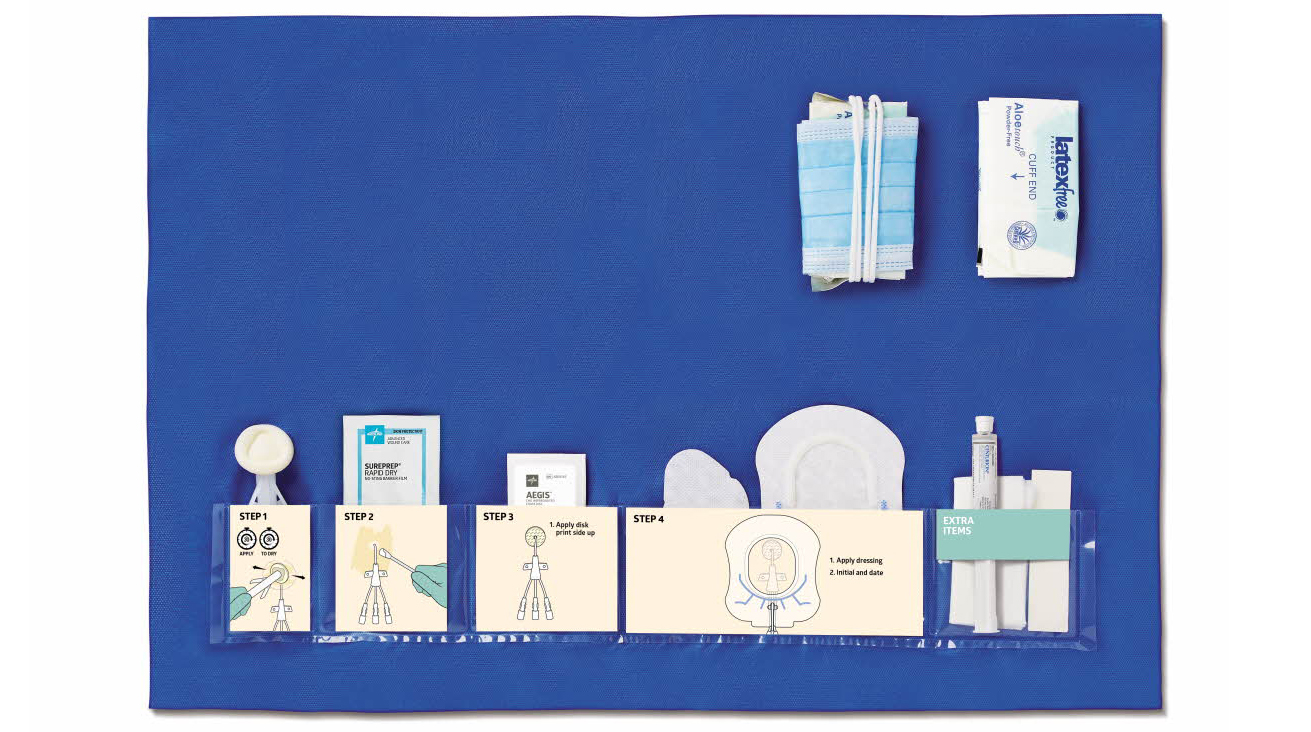
“If you complete the dressing change and you still have stuff left, you didn’t do it right,” Newman says. “If you’re in the process and you’re looking for something else, you didn’t do it the standard way.”
CVC Insertion Kit
CVC insertion and maintenance practices can vary widely based on the products, techniques and precautions clinicians use. In addition, clinician turnover, patient handoffs and competing clinical priorities can create gaps in key areas of care.
CLABSI has a mortality rate of 10 to 25% in US hospitals, leading to as many as 28,000 patient deaths annually in these facilities.2 The good news is, CLABSI’s high mortality rate can be reduced: 65 to 70% of these infections may be prevented by using evidence-based strategies.3
Created by clinicians for clinicians, Medline’s CVC Insertion Kit:
- Provides a systematic approach to CLABSI prevention
- Contains everything clinicians need in the right sequence to minimize variation, enhance clinical workflow and prevent infection
- Addresses each step in the CVC insertion process and specific objectives that must be met to safeguard against infection
- Streamlines the insertion process, letting the team focus on the patient rather than supplies
- Supports post-insertion compliance by providing stabilization and bacterial protection to help prevent dressing disruptions
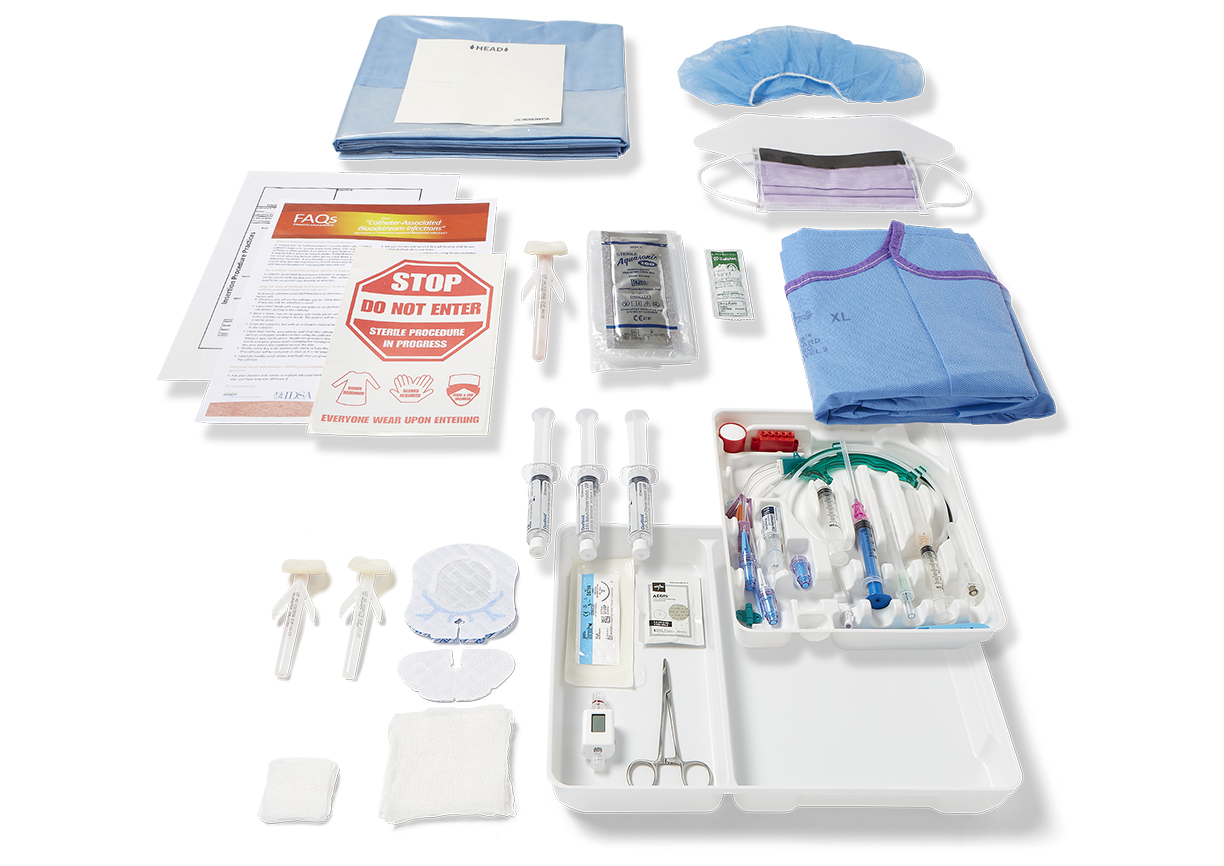
“We need to be mindful that the majority of central lines are in ICUs. There are so many variabilities to the people that have a central line. And the staff that take care of them. We need to make sure that the products and processes don’t have variability,” Matocha says.
The process of refining products based on caregiver feedback takes a significant amount of time, but it’s an essential process to ensure positive outcomes for patients and the success of Medline’s partners, Matocha explains.
“The first run often isn’t the final run,” Matocha says. “This is a process. This is check your ego at the door. This is keep making it better and better until it does what you want to do.”
Empowering clinicians to become innovators and problem-solvers
Medical manufacturers don’t have all the answers to intuitive design. But with the help of physicians, nurses and other practitioners, the industry can move in that direction.
Designers and engineers should closely observe caregivers to ensure their products effectively serve their intended purpose. But manufacturers should also empower clinicians, encouraging them to think creatively about how to improve their day-to-day activities. It doesn’t have to be a complicated surgery or procedure. Improvements to the simplest of processes, such as checking an IV line, can have a notable impact on quality and safety.
Not only should manufacturers embrace caregivers’ feedback, but they should also encourage their ideas and help clinicians turn them into a reality. Clinicians are on the frontlines of quality improvement and cost containment. Manufacturers and healthcare facilities could benefit greatly from their expertise and ambition.
Countless Medline products and solutions have been custom-built for caregiver needs or built on caregiver ideas, said Andy Mills, the company’s president. End-user input and feedback have been and continue to be crucial to the company’s success. That’s why Medline is constantly engaging clinicians to understand their challenges and working with clinicians to create effective solutions.
Key takeaway
Intuitively designed medical products have the potential for immeasurable positive impact on patient outcomes, costs and satisfaction among both patients and caregivers. Clinicians, engineers, designers and manufacturers should be working together to create holistic solutions that take human factors into account. In collaboration with clinicians, Medline has developed intuitively designed kits that help clinicians increase the following of evidence-based best practices, reduce product and process variation, and reduce CAUTI and CLABSI rates.
References:
- Human factors analysis in patient safety systems. (2015, April). The Joint Commission. The Source. 13(4). https://www.jointcommission.org/-/media/deprecated-unorganized/imported-assets/tjc/system-folders/assetmanager/humanfactorsthe_sourcepdf.pdf
- Agency for Healthcare Research & Equity. Central Line-Associated Bloodstream Infections (CLABSI). Accessed 4/11/22. https://www.ahrq.gov/topics/central-line-associated-bloodstream-infections-clabsi.html
- Association for Professionals in infection Control and Epidemiology. (2015). APIC Implementation Guide. Guideline to Preventing Central Line-Associated Bloodstream Infections.