How to engage healthcare leaders in your HAI prevention plan
Use these 5 tips to influence key stakeholders and drive home ROI.

Why is it so difficult to prevent healthcare-associated infections (HAIs)? Because in healthcare facilities, infection can spread through three zones of risk: environment of care, human-to-human transmission or clinical practice. You need resources and support from different teams to fight infection across all three zones.
To successfully drive change, you need to be able to negotiate with and influence key decision-makers.1 Chief among them are senior leaders, such as heads of nursing, quality management and finance.
Hospital leaders play an important role in implementing infection prevention practices and should be engaged at the onset of any program.2,3 However, convincing leaders to invest more money, time and resources in an infection prevention program can be difficult due to a range of complex factors, such as thin margins, pressures to cut costs and competing priorities.
How can you overcome these challenges?
5 tips to engage senior leaders
1 | Understand the economic drivers and their impact
Understanding the external forces that impact an organization’s overall performance can help you understand the priorities of senior leaders and engage with them more successfully.4
“Leaders such as CNOs and CFOs are focused on metrics like outcomes, infection rates, and whether they are meeting value-based purchasing goals to optimize reimbursement,” says Lisa Petrilli, Head of The Medline Institute. “Meanwhile, clinicians working at the bedside are focused on the patients in their care and the processes they’re using to control infection day-to-day.”
The external web of stakeholders who influences infection control programs4
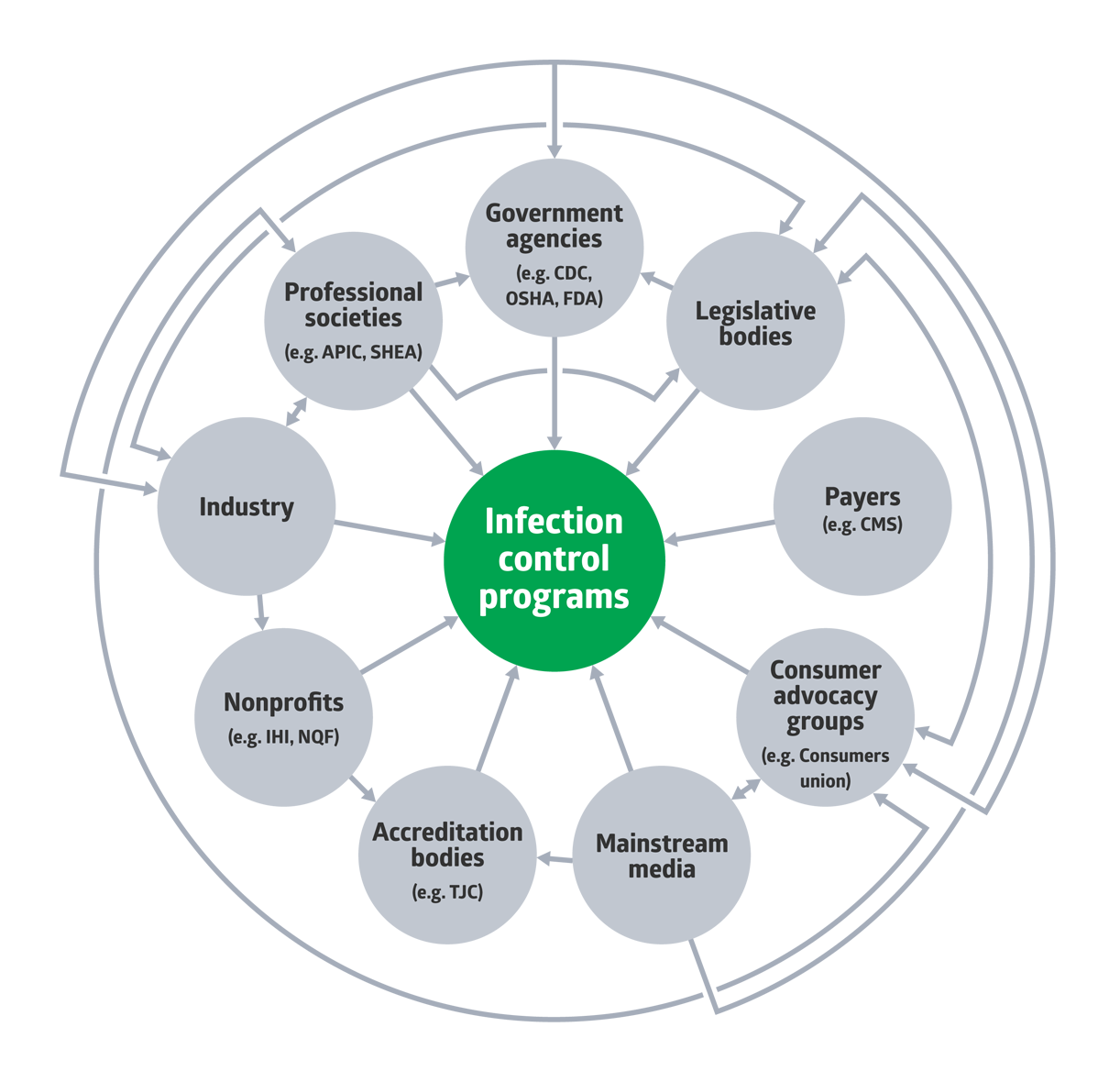
The Centers for Medicare and Medicaid Services (CMS) is one of the key forces within the external landscape, Petrilli points out. The value-based programs they manage can reward or penalize hospitals based on their rates of infection. One example is the Hospital-Acquired Condition (HAC) Reduction Program, which penalizes the worst performing hospitals based on their cases of avoidable healthcare complications, including HAIs like MRSA and C. difficile.
“Through value-based purchasing programs, hospitals are rewarded based on the quality of care they provide and penalized for HAIs,” Petrilli says. “They also don’t get reimbursed when caring for someone with an HAI. Senior leaders are all acutely aware of these things, and if you want to gain their support, it’s important for you to be as well.”

2 | Build a compelling business case
Along with understanding the economic landscape, making a compelling business case is essential to creating a successful IP program, especially in the age of dwindling resources and funding.5,6
When building a case, the Centers for Disease Control and Prevention (CDC) recommends including a financial analysis that demonstrates a return on investment that’s tied to reduced patient harm.6 The oncology unit at one hospital did this and won the support of their executive leadership. Then, upon implementing their intervention, they saw a 65% reduction in central line-associated bloodstream infection (CLABSI) rates.7
“The key is to align the vision you have as an infection preventionist to the needs and priorities of your target audience,” Petrilli says. “When it comes to senior leaders, talk about the return on investment, for example, how your approach can help them reach value-based purchasing goals such as lower infection rates, fewer readmissions or greater patient satisfaction. The Medline Institute has a ‘Leveraging Influence’ seminar that can help you formulate your plan and pitch and develop confidence in your approach.”
The key is to align the vision you have as an infection preventionist to the needs and priorities of your target audience.

Lisa Petrilli
Head of The Medline Institute
3 | Find an executive partner and a team of champions to help make your case
The CDC also recommends identifying executive partners who can advocate for infection prevention goals and share progress with other senior leaders and the hospital board.8 An ideal partner is someone who:
- Has strong communication skills
- Is approachable and willing to commit time
- Is committed to patient safety
- Is respected by their peers
Along with identifying a senior-level advocate, it’s best to find champions among peer groups, according to Angela Newman, Medline Senior Director of Clinical Services. Champions most likely to succeed are those who are already intrinsically motivated and enthusiastic about the practices they promote.9
“Especially if you are new to infection prevention, you need leaders throughout the hospital to help you move the needle,” Newman says.
Team support is critical, given that infection can spread across multiple areas of a healthcare setting. This makes the job of executing infection prevention programs not just the responsibility of the infection preventionist but the responsibility of multiple teams.
“You’re going to need the support of other teams to execute your vision, so it makes sense to find champions early on and leverage them as best you can,” Newman says. “For example, having an infectious disease physician join you in conversations with your CNO can help to show that there is cross-functional support for your ideas, which can help you build a stronger case.”
Especially if you are new to infection prevention, you need leaders throughout the hospital to help you move the needle.

Angela Newman
Medline Senior Director of Clinical Services

4 | Create a focused action plan
Another way to engage leaders is by showing them you have a good action plan.9 Plans should include a clear vision and goal, a timeline and risk analysis, according to the CDC. The organization also advises focusing first on the unit where you are most likely to succeed, then expanding to other areas after demonstrating success.8
Choosing to focus on a specific need or area of opportunity, instead of a large-scale approach, can help make information easier for others to digest and potentially improve odds of success, Newman emphasizes.
“If you know your leader has a lot on their plate, has limited time or often gets pulled in multiple directions, consider narrowing your scope,” Newman says. “You can start that process by identifying the top one or two infection risks to your patient population, whether it’s CAUTI or CLABSI, and using that as a lens to focus your efforts.”

5 | Be sensitive to the challenges teams face
While striving to gain influence, you should at all times remain sensitive to the organization’s culture and “emotional intelligence,” as well as to the many competing priorities that can impact desired clinical and operational outcomes.1 According to Petrilli, showing sensitivity is especially important today, given the new and unique challenges created by the COVID-19 pandemic, from staffing shortages to rising expenses.
“These challenges have created an environment where it’s difficult for anyone to come in and pitch something new,” Petrilli says. “That’s why it’s so important for infection preventionists to emphasize in their plan how it can help teams operate more efficiently or practice infection prevention more easily.”
Key takeaway
You are challenged to work and build consensus across multiple teams. When it comes to engaging senior leadership, you can take actions to more effectively persuade and influence them. The first step is to gain a better understanding of the economic landscape surrounding healthcare. Next is to build a strong business case by showing ROI. While building your case, you should create an action plan with a clearly defined scope and goal. Throughout the process, find peers and executives to partner with as champions, keeping team challenges and limitations top of mind.
References:
- Murphy, D.M., et al. Competency in infection prevention: a conceptual approach to guide current and future practice. American Journal of Infection Control. https://cdn.ymaws.com/www.osap.org/resource/resmgr/Grant_Projects/AJIC_article_Competency_in_i.pdf.
- Centers for Disease Control and Prevention. Strategies for preventing healthcare associated infections. Retrieved August 29, 2021, from https://www.cdc.gov/infectioncontrol/pdf/strive/SP101-508.pdf.
- McAlearney, A.S., et al. Management practices for leaders to promote infection prevention: lessons from a qualitative study. American Journal of Infection Control. https://www.sciencedirect.com/science/article/abs/pii/S0196655320308580
- Weinstein, R.A. Who Is steering the ship? External influences on infection control programs. Clinical Infectious Diseases. https://academic.oup.com/cid/article/46/11/1746/376174
- Dhar, S. et al. Strategies for effective infection prevention programs: structures, processes, and funding. Infectious Diseases Clinics of North America. https://pubmed.ncbi.nlm.nih.gov/34362533/
- Pyrek, K.M. Making the business case for infection prevention. Infection Control Today. https://www.infectioncontroltoday.com/view/making-business-case-infection-prevention.
- Utilizing a business case to link reduction in infections to reduction in costs. (2019, October 10). APIC Industry Perspectives. Environmental Infection. Utilizing a Business Case to Link Reduction in Infections to Reduction in Costs – APIC (industryperspectives.com)
- Centers for Disease Control and Prevention. Creating a business case for infection prevention. Retrieved August 29, 2021, from https://www.cdc.gov/infectioncontrol/pdf/strive/BC101-508.pdf.
- Saint, S. and Greene, M.T. Preventing CAUTI: engaging clinicians and senior leadership to implement change. Agency for Healthcare Research and Quality: https://www.ahrq.gov/hai/cauti-tools/archived-webinars/preventing-cauti-engaging-leadership-slides.html




