Harness the power of UV light disinfection to fight pathogens
Target air and surfaces with UVC technology.

Minimizing the spread of harmful pathogens is your everyday challenge. Even now, COVID-19 risk remains and the threat of superbugs is ever present. The difficulty is real—surface-dwelling bacteria like MRSA and C. difficile spores can cling for months to hard surfaces like tables, railings and floors.1 And pathogens causing pneumonia, tuberculosis, influenza and others can linger in the air from minutes to hours.
What can you do? Consider adding ultraviolet disinfection to your EVS team’s cleaning and disinfection program. This powerful supplement is an important part of a comprehensive strategy to eliminate harmful pathogens and keep people safe.
UV technology isn’t new, but can be confusing
Today, UV technology is widely used in healthcare—for fast disinfection of handheld devices, robotic disinfection of room air and surfaces, and for air disinfection via UV elements in heating, ventilating and air-conditioning (HVAC) systems. But despite UV’s wide use, misconceptions about it abound.
In fact, with no established industry standards for certification, false or misleading claims about efficacy and safety can occur. And with so many devices, capabilities and price points, it’s not easy to know what’s best for your facility.
Let’s clear up the confusion about UV disinfection so you can make good decisions, starting with the basics.
What is UV light?
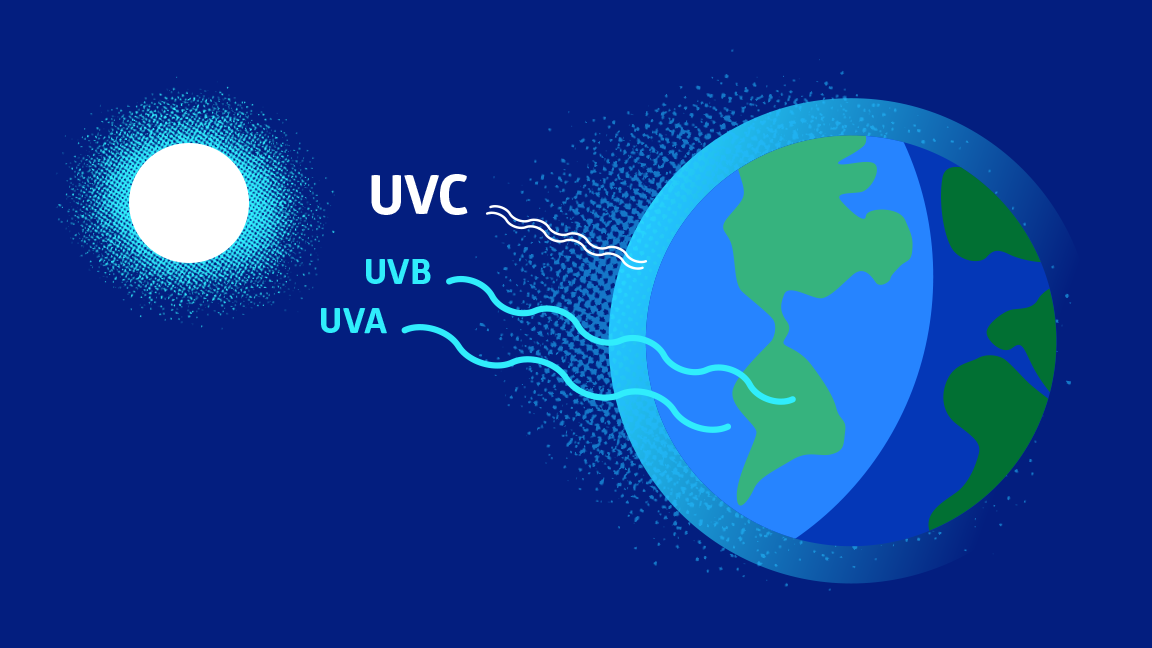
UV light is a type of electromagnetic radiation produced naturally by the sun and transmitted in wavelengths measured in “nanometers” or billionths of a millimeter.
The long and short of UV measurements
UVA and UVB rays are known for their ability to tan, or harm, human skin and eyes. The UVC range has the most powerful germicidal properties, specifically at the 254nm wavelength.
- UVA—long wave, suntanning range (315-400 nm)
- UVB—medium wave, sunburning range (280-315 nm)
- UVC—short wave, pathogen-killing range (200-280 nm)
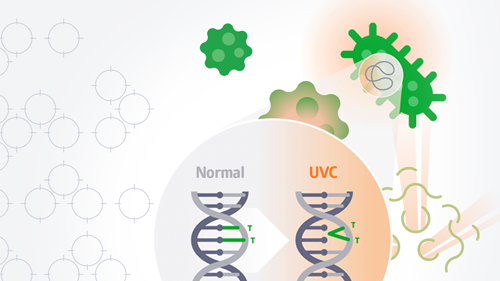
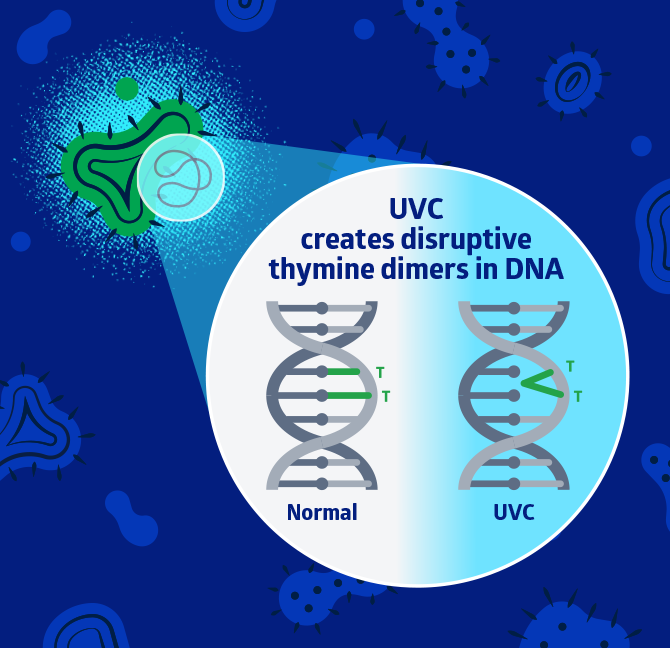
How does UVC light fight bacteria and viruses?
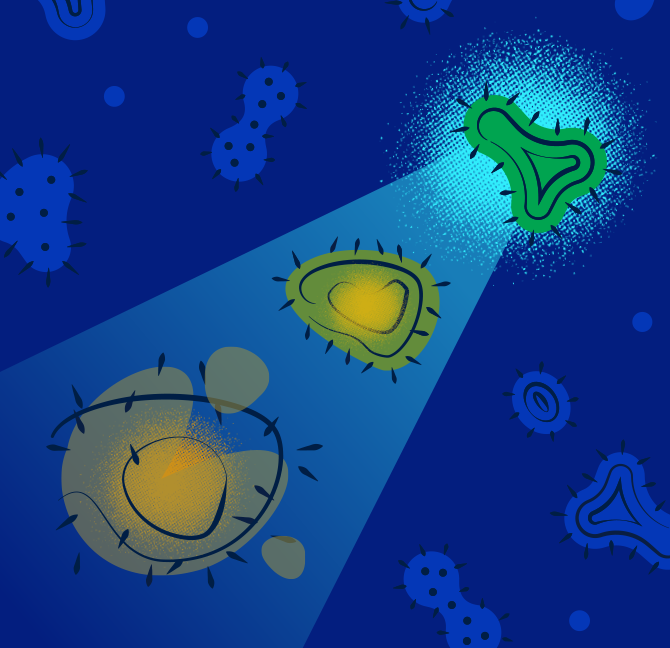
When UVC is emitted at certain wavelengths for specific amounts of time, it’s absorbed by bacterial and viral cells, damaging their DNA and RNA. That disrupts cellular repair and reproduction and effectively inactivates or kills the cell.
Low doses can inactivate a pathogen. Recommendations vary by device and factor in the intensity of the light source, the distance from surfaces and length of exposure. Higher intensity sources use shorter exposures. Lower intensity sources use longer exposures.
UVC light vs germs
- 99.99%+ efficacy vs coronavirus 2,3
- 99.99%+ efficacy vs super bugs including MRSA and C. difficile 4,5
What are the types of UVC light technology and how do they work?
Pulsed xenon and mercury gas bulbs are the two main types of UVC technology. Both disinfect the air and surfaces, but they kill or disrupt pathogens in different ways.
Low-pressure mercury gas bulbs
- Most common UVC disinfection source
- Emits 254nm UVC wavelengths, the most effective pathogen-killing level, in a continuous stream
- Stops pathogen cell reproduction and kills cells when at higher dosages
- Devices typically cost less than PX-UV sources
Pulsed xenon (PX-UV)
- Emits high-intensity germicidal UVC (100-280 nm) and visible spectra (380-1000 nm) in short, high-intensity pulses
- UVC disrupts pathogen cell reproduction and broad spectrum light heats cell until it ruptures
- Devices are typically more expensive than mercury gas bulb sources
What are the different types of UVC devices?
- Both mercury gas and pulsed xenon UVC-emitting robots or devices can disinfect surfaces and air in entire rooms. Some devices can kill pathogens on hard surfaces in 5 minutes while simultaneously disinfecting 250 cubic feet of air per minute (CFM).
- UVC mobile cabinets offer rapid disinfection for smaller, high-touch items like tablets, cellphones and stethoscopes and may kill pathogens in as few as 30 seconds.
- Portable UVC air disinfection devices stop smaller pathogens that HEPA filtration can miss. They can achieve efficacy of 99.9% against airborne mold and Cladosporium cladosporioidem, and 99.99% against bacteria including C. difficile, MRSA and others.7 Some combine HEPA, UVC and carbon filters to disinfect and deodorize the air.
Are UVC disinfection devices harmful to people?
Both mercury gas and pulsed xenon are safe when manufacturer instructions are followed. Surface disinfecting devices are typically used in an unoccupied room. UVC light can cause temporary skin and eye discomfort if above NIOSH safe exposure limits, so workers should avoid looking at UVC light. UVC does not penetrate through ordinary glass, so anyone behind a window is protected.8
Does UVC light damage and degrade healthcare equipment and surfaces?
UVC light’s short wavelength can’t penetrate deeply enough into surfaces to affect equipment function or surface integrity.8
Is manual cleaning and disinfection needed if UVC is used?
UVC light is an excellent supplement to manual cleaning, with the two working hand-in-hand.
Because UVC’s short wavelengths can’t penetrate soil and liquids, manual cleaning with chemical disinfectants should remove those first. Manual cleaning is also needed for areas where the UVC light can’t reach. But UVC light effectively kills pathogens manual cleaning misses. Studies show that inconsistent product use and manual cleaning practices can result in just half of targeted surfaces being disinfected. UV fills the gap.8
How can you find the right UVC light system to meet your needs?
- Look for a versatile UVC light disinfection system that offers a high kill rate of airborne and surface pathogens.
- Compare room disinfection times and dosages for different light sources to determine the best value for your facility. Sometimes faster devices come at a high cost, though efficacy may be the same.
- Check out claims. Many speed and efficacy claims are based on testing at minimal distances—even as close as 1 foot. Real-world testing should be at least in the 5-15 feet range.
Key takeaway
UVC light can quickly and effectively disinfect surfaces and air in patient rooms, operating rooms and lobbies; and on high-touch equipment like tablets and stethoscopes. It’s an excellent supplement to your EVS team’s manual cleaning and disinfection efforts. Low-pressure mercury gas bulbs and pulsed xenon UVC technologies each have different qualities. Consider your uses and budget, and check efficacy claims and testing methods to determine which UVC devices are best for your facility.
References:
- Suleyman, G., Alangaden, G. & Bardossy, A.C. The Role of Environmental Contamination in the Transmission of Nosocomial Pathogens and Healthcare-Associated Infections. Curr Infect Dis Rep. 2018;20:12. Available at: https://doi.org/10.1007/s11908-018-0620-2. Accessed October 1, 2021.
- Zargar et al., Assessment of LYTBOT to reduce pathogens on nonporous and porous surfaces: Testing with Human Respiratory Coronavirus 229E (ATCC VR-740), CREM Co. Labs. December 11, 2020. (Testing Organism: Human Respiratory Coronavirus 229E (ATCC VR-740), Host: MRC-5 cells (ATCC CCL-171)
- Christiane Silke Heilingloh PhD, et. al. Susceptibility of SARS-CoV-2 to UV irradiation, Am J Infect Control. 2020 Oct;48(10):1273-1275. doi: 10.1016/j.ajic.2020.07.031. Epub 2020 Aug 4. https://pubmed.ncbi.nlm.nih.gov/32763344/. Accessed April 29, 2021.
- Lo et al., Disinfection Effifi ciency Study of a Pulsed Light System, Mount Sinai Hospital. April 1, 2016.
- Lighthouse Healthcare Partners website, https://www.lhhcp.com/solaris, accessed April 16, 2021.
- Alberts B, Johnson A, Lewis J, et al. Molecular Biology of the Cell. 4th edition. New York: Garland Science; 2002. DNA Repair. Available from: https://www.ncbi.nlm.nih.gov/books/NBK26879/. Accessed November 17, 2022.
- Data on file.
- https://industryperspectives.com/wp-content/uploads/2021/09/UV_Fact_vs._Fiction_Whitepaper_MKTFM_687_Rev_A.pdf, page 8, Accessed October 31, 2022.