You can stop nursing home infections even with staffing issues
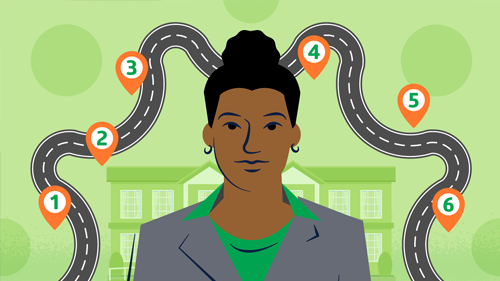
5 ways to prioritize HAI prevention—and encourage staff to stay.

In long-term care (LTC), you face unique challenges when it comes to preventing healthcare-associated infections (HAIs). Facility residents are at higher risk of infection,1 financial resources are limited and staffing shortages are a constant worry.
In fact, a recent survey shows that 84% of nursing homes are experiencing moderate to high staffing shortages, and 94% are having trouble hiring staff.2
So how do you protect residents, staff and visitors from the spread of pathogens? By being firm in your commitment to following best practices and flexible in your approach. Here’s how.
1
Gain the knowledge you need to lead.
Does your facility have a solid, broad infection prevention and control (IPC) program in place? That’s where to start. When you have carefully developed protocols and processes, you can educate staff, residents and their family members. A short risk assessment can help you identify gaps.
Maybe you’re new to IP. As early as you can, make sure to take the free specialized training offered by the Centers for Disease Control and Prevention (CDC).3 And look to your director of nursing and other experts for direction and insights.
When you feel confident in your expertise, you’re better equipped to share best practices throughout your facility. And staff will look to you as a go-to person for guidance.
2
Provide pre-work and competency assessments to agency nurses.
Like other LTC facilities, yours is using agency nurses to fill staffing gaps. How much do you know about them before they start?
A quick way to help agency nurses prepare is to give them pre-work. You can send them quizzes to help identify gaps in knowledge related to infection prevention. Do you have brief videos to share? They should cover the basics: hand hygiene and personal protective equipment.
If you don’t have these pieces available, your medical supplier may be able to provide videos and other online education, as well as help with training.
84% of nursing homes
are experiencing moderate to high staffing shortages2
3
Make the most of part-time employees.
Your full-time staff probably have consistent schedules, with part-time staff filling in gaps. A recent study found that scheduling practices for part-time workers such as certified nursing assistants (CNAs) can drive poor consistency of care in LTC facilities. Researchers concluded that prioritizing consistent scheduling for these workers can significantly improve consistency of care, which is associated with better quality of life for both residents and workers.4
“A consistent schedule for part-time workers helps them build relationships with the residents they’re providing care for,” says Caryn Arnold, MBA, RN, BSN, CNOR(E), a-IPC, Medline Medical Science Liaison. “It also enables staff to find informal mentors on their shifts.”
Consistency in scheduling can benefit full-time staff as well. They get to know the part-time staff and their capabilities, as well as areas they could use guidance. And your facility is better positioned to ensure that someone with IP knowledge is available on every shift.
4
Be flexible with scheduling.
It’s not just part-time staff who need attention. When LTC nurses working full-time shifts were interviewed about scheduling practices, they flagged issues such as switching caregivers between day and night shifts frequently and unpredictably; only offering eight-hour rather than longer shifts; and demanding on-call hours tacked onto already long shifts.5
Can your facility give nurses the hours they want? Are 10-hour or 12-hour shifts possible? How about 6-hour shifts?
“Maybe some nurses don’t want to put their kids in daycare before and after school,” says Arnold. “A nine to three shift will meet their needs.”
Make family caregivers feel welcomed, empowered and appreciated.

Caryn Arnold, MBA, RN, BSN, CNOR(E), a-IPC
Medline Medical Science Liaison
Nurses will appreciate any flexibility possible. They’ll be better rested, have better work-life balance and be better able to stay on top of infection prevention practices. In addition, they’ll be more likely to stay.
5
Incorporate informal caregivers into your care team.
LTC residents often have family members or other caregivers helping them throughout the day. Researchers at the University of Pennsylvania said LTC facilities should better incorporate informal caregivers to enhance professional caregivers’ capabilities and efficiencies.6
For example, researchers found that 75% of nursing home residents needing help with mobility had those needs met by informal care providers. The researchers suggested that family caregivers could be integrated into a resident’s care team in several ways, including through formal training and the adoption of more explicit integrated care models in which formal and informal care providers cooperate.
How can your facility take advantage of this “invisible workforce”?
“Make family caregivers feel welcomed, empowered and appreciated,” says Arnold. “Even if they helped their loved ones before a long-term care facility was needed, they may feel intimidated or unneeded once they’re surrounded by professional caregivers.”
Let’s say a resident has mobility issues and needs help getting out of bed or dressing. A family caregiver can be shown how to provide the assistance correctly, so that neither the resident nor the caregiver is at risk of injury.
What about when family members help residents with hand hygiene? Residents and their loved ones need education on when and how to properly clean hands. Family caregivers also should be educated on when and how they should wear PPE when assisting their loved ones.
In addition, family caregivers can help move items off of tray tables and other surfaces so environmental services staff are able to clean and disinfect regularly.
“When family caregivers are provided training on how to safely help their loved ones, they’ll view your facility as a safer place,” says Arnold.
Key takeaway
Long-term care facilities face numerous challenges when it comes to infection prevention, including ongoing staffing shortages. By arming yourself with knowledge, making the most of part-time staff, showing more flexibility with full-time staff and incorporating informal caregivers into your workforce, you can enhance the culture of safety in your facility—and make staff want to stay.
To enhance your hiring practices, check out the Careers in Caring campaign launched by the American Health Care Association and the National Center for Assisted Living.7
References:
- Agency for Healthcare Research and Quality. (2017, March). A Unit Guide to Infection Prevention for Long-Term Care Staff. https://www.ahrq.gov/sites/default/files/wysiwyg/professionals/quality-patient-safety/quality-resources/tools/cauti-ltc/modules/resources/guides/guide-infection-prevention.pdf
- American Health Care Association. (2023, January). State of the Nursing Home Industry. State of the Nursing Home Industry | Dec 2022 Survey (ahcancal.org)
- Nursing Homes and Assisted Living (Long-Term Care Facilities [LTCFs])/Infection Prevention Training. Retrieved March 15, 2023, from Infection Prevention Training | LTCF | CDC.
- Carnegie Mellon University. (2022, December 20). For LTC Facilities, Prioritizing Part-time Employees Can Boost Consistency of Care. Healthcare Hygiene Magazine. For LTC Facilities, Prioritizing Part-time Employees Can Boost Consistency of Care—Healthcare Hygiene magazine
- Deng, Wei. (2022, July 18). To address the staffing crisis in LTC, start with scheduling. McKnight’s Long-Term Care News. To address the staffing crisis in LTC, start with scheduling—Marketplace Experts—McKnight’s Long-Term Care News (mcknights.com)
- Brown, Danielle. (2022, January 6). Researchers call for family caregivers to be better incorporated into nursing home workforces. McKnight’s Long-Term Care News. Researchers call for family caregivers to be better incorporated into nursing home workforces—News—McKnight’s Long-Term Care News (mcknights.com)
- AHCA/NCAL. (2023, January 11). Careers in Caring. Careers in Caring—A Long Term Calling (careersincare.org)