Optimizing catheter care by CNAs and other non-clinicians
Any activity that involves patient movement creates risk of a CAUTI.

A hospital nurse determines that a patient needs an indwelling urinary catheter, or Foley. Following best practices, the nurse inserts the Foley catheter for a patient. Everything is in the right place, and the patient is resting comfortably. No need to worry about catheter-associated urinary tract infections (CAUTIs), right?
But the patient is scheduled for multiple activities that day: physical therapy, an MRI and a surgical procedure. These events involve patient movement and/or transport—and the potential for causing a CAUTI to develop.
“Everyone in a hospital who has any patient contact can contribute to or help prevent CAUTIs,” says Mary Pat Eble, MSN, RN, Medline National Clinical Product Specialist, Urology. “Ancillary team members know that a Foley catheter helps drain urine. But they need to understand the basic mechanisms of the catheter to ensure it continues to function properly.”
What a properly functioning Foley catheter looks like
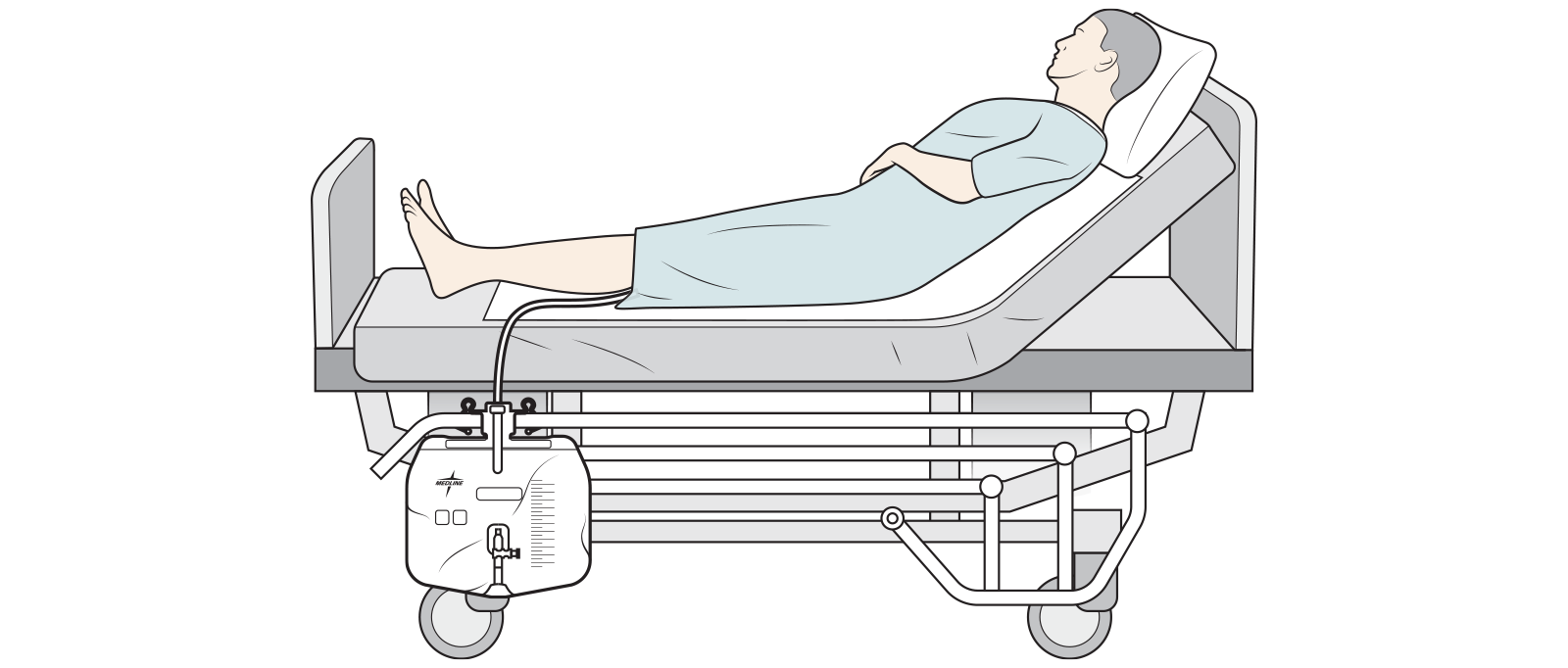
- The catheter is secured and the drainage system is closed to protect from germs entering and causing infection.
- The urine drain bag is below the level of the patient’s bladder to prevent backflow.
- The catheter tubing is free of kinks to prevent obstruction of urine flow to the drain bag.
- The catheter tubing does not contain any dependent loops, which is when looped tubing falls lower than the urine drain bag.
- The urine drain bag is not on the floor or on top of the patient’s legs/feet.
Ancillary team roles in maintaining proper catheter function
While different team members have specific roles and responsibilities, all team members should: Perform hand hygiene immediately before and after handling the catheter or drainage system, and use clean gloves while handling the catheter or drainage system.
Certified nursing assistants (CNAs)

CNAs don’t insert catheters, but they do assist with catheter maintenance. The Agency for Healthcare Research and Quality (AHRQ) recommends the following seven practices:
- Perform perineal care using only soap and water or a similarly gentle cleaning agent.
- Keep the catheter and tubing from kinking and becoming obstructed.
- Keep the catheter drainage system closed when using the urine drain bag.
- Replace the whole system (catheters and urine drain bags) if there is a break in the system.
- Ensure the patient’s identifier and implementation date is on their urine drain bag emptying containers.
- Disinfect the sampling port before obtaining a sample.
- Empty the urine collection bag before a patient is moved or transported.1
5% increase of CAUTI
in US hospitals between 2020 and 20212
Physical therapist/Occupational therapist

Before getting started, PTs/OTs should have the nurse or CNA empty the drainage bag.
Then, either the patient or the therapist should coil the tubing and hold it with the drain bag in their hand below the level of the bladder. If the patient has a walker, it’s acceptable to coil the tubing and hang it on the lower bar of the walker, making sure the tubing and drain bag are not resting on the floor and causing a tripping hazard for the patient.
It’s ideal to have two people providing the therapy, but that’s not always possible with staff shortages. The good news is, patients’ families are some of the best caregivers. They just need direction on how they can help and what they can do.
Transporter/OR technician

“There are challenges moving a patient and their devices onto and off of a gurney,” says Donna Matocha, DNP, MSN, VA-BC, Medline Manager of Clinical Resources – Acute Care. “You don’t want the catheter to get pulled out or cause any trauma due to tugging on the securement device.”
Techs should examine the catheter setup before moving the patient. First, it’s important to make sure the catheter is secure, because if it’s not, all that movement is going to cause the catheter to slide in and out, which can increase the likelihood of allowing in bacteria extraluminal. And it can cause irritation, both of which could lead to a CAUTI.
Then, they should follow the tubing down and check to see if there is anything obstructing it.
Before moving a patient onto a gurney, the transporter or OR tech should have the drainage bag emptied by a nurse or CNA.
The drainage bag should be moved before the patient and hung at the foot of the gurney.
Imaging/Lab technician

“Most imaging areas should have either an IV pole that has a hook on it or a stool with a high bar to assist staff in positioning patients on the CT or MRI table,” says Eble. “They should have some piece of equipment they can hang the drain bag on so it is below the level of the bladder and does not have any dependent loops during imaging. They should not put the drain bag on the patient’s legs.”
Once the tech knows where on the MRI equipment the patient is going to be, the tech could hang the bag on the table itself. But only if the table is not going to be sliding in and out, possibly breaking the hook, tugging on the catheter and possibly causing the catheter to be dislodged.
Educate and provide tools for team members
Everyone works best when they understand why they’re supposed to—or not supposed to—do something. Consider having staff view a video that shows what happens when best practices aren’t followed.
Conduct in-services and provide posters that show the right position and location of the whole catheter system. Staff will then be aware of how they can help prevent CAUTIs with every patient contact.
Key takeaway
Everyone who comes in contact with a patient plays a role in preventing healthcare-associated infections (HAIs) such as CAUTIs. By educating staff on what they need to do and why, you can help them carry out their roles effectively and increase patient safety.
References:
- AHRQ. (2017, March). Catheter Care Do’s and Don’ts. Catheter Care Do’s and Don’ts | Agency for Healthcare Research and Quality (ahrq.gov)
- Centers for Disease Control and Prevention. (2021, November 4). Healthcare-Associated Infections / Current HAI Progress Report / 2021 National and State Healthcare-Associated Infections Progress Report. Current HAI Progress Report | HAI | CDC