Central line care: Use the right dressing and securement
Explore ways to prevent CVC dislodgement and dressing disruption.
You work hard to prevent healthcare-associated infections (HAIs), as shown by gains in HAI reductions in the five years before the COVID-19 pandemic hit. Did you know that central-line associated bloodstream infection (CLABSI) rates decreased by 31%?1
Unfortunately, CLABSIs in US hospitals are on the rise, increasing 28% in 2020, compared to 2019.1 This complex HAI can have significant consequences. For example, CLABSI:
- Has a mortality rate of 10 to 25% in US hospitals
- Is associated with significant morbidity and costs
- Leads to as many as 28,000 patient deaths annually in US hospitals2
What can be done to bring those rates back down?
The key is using the right products and processes for central venous catheter (CVC) insertion and management. Throughout the life of the line.
What are the major risk factors?
CVCs provide entryways and breeding grounds for germs that can lead to CLABSIs. Catheter securement and dressings are vital to keeping the entryway sterile:
- Securement devices are applied to prevent the CVC from becoming dislodged
- Dressings cover the insertion site and help prevent infections from starting; they also help prevent the CVC from moving around
However, even when a securement/stabilization device is applied at insertion, CVCs can become dislodged from strong tugging forces or loose securement.3 In addition, central line dressings should remain securely in place for seven days, but a study demonstrated that 67% of CVC dressing changes were unscheduled due to disruptions—failing in their attempt to protect patients from bloodstream infections.4
That’s why central CVC dislodgement and dressing disruption are major risk factors for CLABSIs. Let’s take a look at how proper catheter securement/dressing selection and management can help you prevent CLABSIs.
Recommended securement solutions and practices
During 2001-2002, the Institute for Healthcare Improvement (IHI) became a pioneer in the field of CLABSI reduction when it introduced its first bundle of prevention practices. The IHI defines a bundle as a “small set of evidence-based interventions for a defined patient population and care.”
The CLABSI bundle identified a group of interventions supported by the highest level of research which, when used together, would ideally produce better outcomes than if one or more had been used separately. The practices described in the IHI CLABSI insertion bundle include:
- Hand hygiene
- Maximal sterile barrier precautions upon insertion
- Chlorhexidine skin antisepsis
- Optimal site selection (avoidance of femoral vein in adults)
- Daily review of central line necessity and prompt removal of unnecessary lines5
For securement, the 2021 INS Infusion Therapy Standards of Practice recommend using a catheter-specific and sutureless securement device to reduce risks of catheter dislodgement.6
“When sutures are tugged, they pinch and pull,” says Donna Matocha, DNP, Medline Manager of Clinical Resources–Critical Care. “They’re a source for biofilm formation and can become infected. The other big push initially to get rid of sutures was by OSHA due to needlestick injuries.”
Sutures aren’t recommended, so your securement device should prevent common contributors to CVC dislodgement. These include loose securement, patients removing CVCs, patient activities in bed, walking, staff assistance with activities and transfers from bed.3
“Patient repositioning, physical therapy, being transported for tests or anytime the patient moves or is being moved—these all cause tugging,” says Matocha.
“When sutures are tugged, they pinch and pull. They’re a source for biofilm formation and can become infected.”

Donna Matocha, DNP
Medline Manager of Clinical Resources—Critical Care
How do you define an effective securement device? One that:
- Provides secure hold, resisting multi-directional tugging forces
- Has deep notches to keep tubes in place
- Maintains securement by flexing with patient movement
- Has soft fabric that conforms with skin movement
“For some securement devices, you have to use a skin prep, making sure to let it dry after application,” says Matocha. “You can’t put it on a wet surface, and you can’t put it on a dirty surface. It’s like bandaging a wound on dirty skin.”
Insertion site dressings that protect CVCs and patients
Dressings cover and protect insertion sites, helping to prevent infections. They should stay on securely for up to seven days. Premature dressing changes, or dressing disruption, are performed immediately if the dressing becomes damp, loosened or visibly soiled; or if moisture, drainage or blood are present under the dressing.7
Frequent dressing changes can cause damage to the surrounding skin and increase the potential for infection. In fact, a study demonstrated that more than two dressing changes for disruption were associated with a higher than three-fold increase in the risk of CLABSI. When the final dressing is disrupted, the risk of catheter colonization or infection is increased by more than 12-fold.4
65 to 70% of CLABSIs
may be prevented by using evidence-based strategies5
An effective dressing has:
- Soft fabric that conforms with skin movement
- Contoured edges to help prevent dressing from peeling up
- Protective film barrier to help keep pathogens away from the insertion site
- Absorbent pad to wick away moisture
- Large transparent window for thorough site assessment
Prevalence rounds should be conducted to ensure dressings are fully intact—all four corners.7
Today’s innovative options
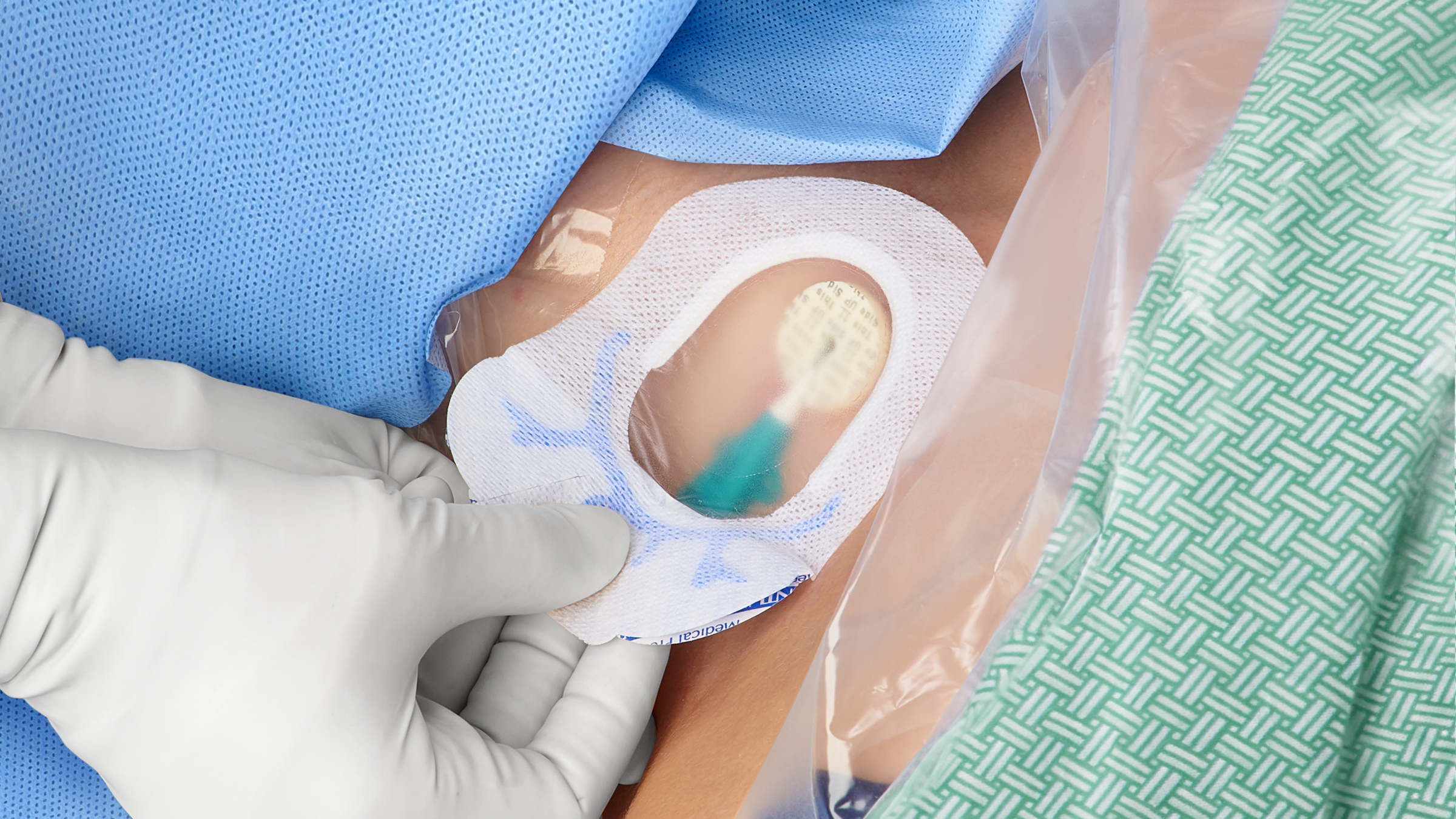
Look for integrated CVC dressings that combine barrier protection, catheter securement and site visibility that enables monitoring of the CVC and insertion site. Security is provided via an integrated anchor that’s built into the product, helping prevent tugging forces from reaching the insertion site.
A one-step dressing and securement device is designed to stay firmly in place for up to seven days. An integrated product helps make the dressing removal process a lot simpler and more comfortable for patients, some of whom have fragile skin.
Maintenance bundles help improve care
CVC post-insertion (maintenance) bundles for securement devices and dressings are becoming more widespread. They may include elements such as:
- Daily review of line necessity with prompt removal of unnecessary CVCs and documentation
- Details of removal documented in the records
- Hand hygiene before manipulation of the IV system
- Catheter injection ports
- Proper procedures for catheter site dressing monitoring/changes
- Catheter access/manipulation
- Administration set (primary and secondary) replacement
- Intravenous fluid preparation using aseptic technique
- Healthcare personnel training8
These bundles have been shown to result in vein preservation, improved patient experience, increased nursing efficiency, fewer skin breaches and reductions in materials costs.
Finally, your healthcare facility should have a vascular access specialist team that has advanced knowledge when it comes to insertion techniques, clinical care and management of vascular access devices.
Key takeaway
CLABSI rates have been increasing since 2020. CVC dislodgement and dressing disruption are major risk factors for this HAI with mortality rates up to 25%.2 Selecting and appropriately using the right securement devices and dressings—and employing insertion and maintenance bundles—will help reduce CLABSI rates, increase patient safety, prevent longer lengths of stay and reduce costs.
References:
- Patel, Prachi; Weiner-Lastinger, Lindsey; Dudeck, Margaret; et al. Impact of COVID-19 pandemic on central-line-associated bloodstream infections during the early months of 2020, National Healthcare Safety Network. Infect Control Hosp Epidemiol. 2021 Mar 15;1-4.
- Agency for Healthcare Research & Equity. Central Line-Associated Bloodstream Infections (CLABSI). Available at: https://www.ahrq.gov/topics/central-line-associated-bloodstream-infections-clabsi.html. Accessed 4/11/22.
- Moureau, Nancy. Impact and Safety Associated with Accidental Dislodgement of Vascular Access Devices: A Survey of Professions, Settings, and Devices. Journal of the Association for Vascular Access, Volume 23, Issue 4, December 2018, Pages 203-215.
- Timsit, Jean-François; Bouadma, Lila; Ruckly, Stéphane; et al. Dressing disruption is a major risk factor for catheter-associated infections. Crit Care Med. 2012 Jun;40(6):1707-14. Available at: https://pubmed.ncbi.nlm.nih.gov/22488003/
- APIC Implementation Guide. Guideline to Preventing Central Line-Associated Bloodstream Infections. 2015.
- Gorski, Lisa. A Look at the 2021 Infusion Therapy Standards of Practice. Home Healthcare Now, March/April 2021, Vol 39, Number 2, pp 62-71.
- DeVries, Michelle. Addressing the Dressing: Improving Dressing Disruption in Vascular Access presentation. 2018.
- The Joint Commission. Preventing Central Line-Associated Bloodstream Infections: Useful Tools, An International Perspective. November 20, 2013. Available at: https://www.jointcommission.org/-/media/tjc/documents/resources/clabsi/clabsi_toolkit_tool_3-22_cvc_maintenance_bundles.pdf. Accessed April 11, 2022.




