Hospital switches to hybrid underpad program and saves thous
Fawcett Memorial Hospital moves from one-size-fits-all approach, reducing cost and waste.

Insight
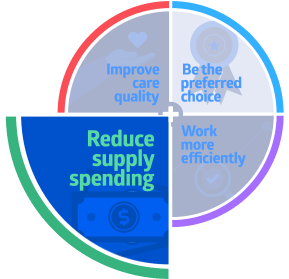
Our mission is to make healthcare run better by improving operating performance in four key areas. This is how we help bring down overall costs, as well as protect and grow revenue.
In this case study, we focus on reducing supply costs through more effective utilization. Healthcare providers need reliable and cost-effective incontinence products to protect patients from skin damage caused by excess moisture. Most hospitals take a one-size-fits-all approach, using a single category—for example, high-end disposable underpads—which can lead to overspending.
We helped Fawcett Memorial Hospital evaluate its moisture management needs against best practice benchmarks. Next, we created a blended, more cost-effective program of disposable and reusable underpads based on different levels of patient need. The result: better financial outcomes, without compromising patient care.
Challenges
- Overspending on moisture management program
- Maintaining patient skin care
Actions
- Assess spend/utilization against best practice benchmarks
- Evaluate different products and determine clinical benefits
- Develop hybrid product formulary customized to patient needs
Results
- Maintained skin health without compromising care
- More than $50,000 a year in supply cost savings
- Reduced waste
Challenges
Healthcare providers encounter many different skin conditions every day. But among the most common are those caused by prolonged exposure to moisture, including incontinence associated dermatitis (IAD).
IAD is characterized by inflammation of the skin caused by exposure to urine or stool. Skin breakdown resulting from IAD and other moisture-associated skin damage is a common, costly and painful problem. Patients with both incontinence and impaired mobility are at a 37.5% greater risk of developing a pressure injury.1 Approximately 60,000 patients die from pressure injuries each year.2
Healthcare providers require reliable and cost-effective solutions to protect against IAD. Though available incontinence products vary in design and cost, most fall into one of two categories: disposable, fast-drying premium or reusable, breathable underpads.
60,000
Approximate number of patients that die from pressure injuries each year2
Comparing options
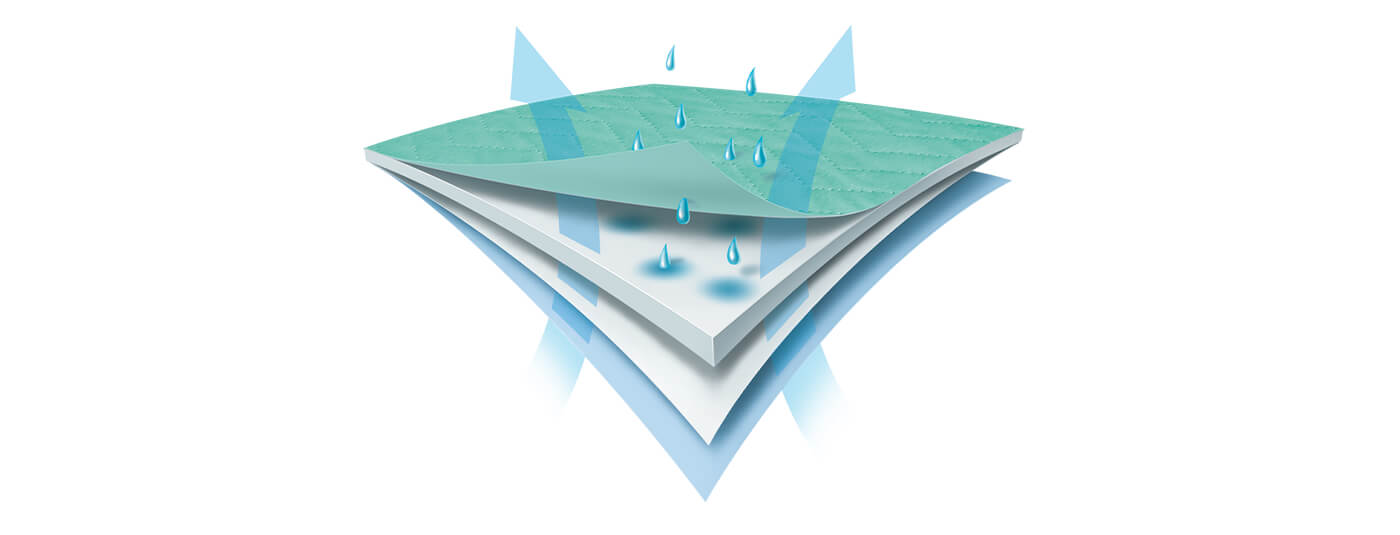
Both types of underpads offer benefits for healthcare facilities. Disposable, fast-drying premium underpads—can be relatively expensive, but they contribute to better skin outcomes when used for high-moisture, high-fluid-output incontinence care. By drawing in moisture and locking it away from the skin, premium drypads maintain skin integrity in patients and reduce the risk of hospital-acquired pressure injuries.
Key benefits of disposable premium underpads:
- Dry to the touch in minutes
- Breathable for skin health and patient comfort
- Lies flat when wet, without bunching, swelling or disintegrating
- Maintaining proper pressure index
- Managing multiple voids
In contrast, reusable underpads are often less expensive, helping decrease waste and cost. Though they don’t dry as quickly as disposable dry underpads, innovations are changing that. Reusable options are best for noncritical patients because they are less likely to have high-fluid incontinent episodes during their hospital stays.
Benefits of reusable underpads:
- Tolerating multiple washings
- Breathable for skin health and patient comfort
- Lying flat when wet, without bunching, swelling or disintegrating
- Maintaining proper pressure index
- Helping reduce waste and costsMany US hospitals utilize one of these options exclusively to manage incontinence. Fawcett Memorial was using 100% disposable underpads and overspending on its moisture management program.
Many US hospitals utilize one of these options exclusively to manage incontinence. Fawcett Memorial was using 100% disposable underpads and overspending on its moisture management program.
Actions
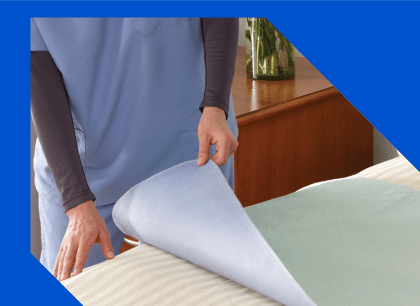
Brenda Sellers, RN, Clinical Resource Director at Fawcett Memorial, was interested in taking a hybrid approach to the hospital’s incontinence products, using disposable drypads for high-risk patients and reusable options for noncritical patients. This type of blended moisture management solution makes the best use of both underpad options: cost-effective reusable and fast-drying disposable.
Results
$50,000
Amount saved in supply costs with the introduction of reusable pads
Sellers led a clinical trial to determine the correct ratio of reusable and disposable underpads Fawcett needed. Based on the findings, Fawcett switched to the hybrid approach, using 75% breathable, reusable underpads and 25% dry, disposable underpads.
The introduction of a reusable pad saved Fawcett more than $50,000 a year in supply costs and significantly reduced waste—all without any negative impact to patient skin health.
References:
- Langemo D, Hanson D, Hunter S, et al. Advances in skin & wound care. The Journal for Prevention and Healing. 2011;24(3):126-140. Available at http://www.nursingcenter.com/cearticle?tid=1130247#P181 Accessed March 13, 2020.
- Preventing pressures ulcers in hospitals. Agency for Healthcare Research and Quality. Available at: https://www.ahrq.gov/patient-safety/settings/hospital/resource/pressureulcer/tool/pu1.html. Accessed March 13, 2020.
Please complete the form to receive additional content when published.
References
- Learn more about abaqis here.
- Discover more ways we’re helping providers make healthcare run better.
- See abaqis in action.
How can we help your business run better?
Contact us to learn more