Stay ahead of PIs with this first-of-its-kind dressing
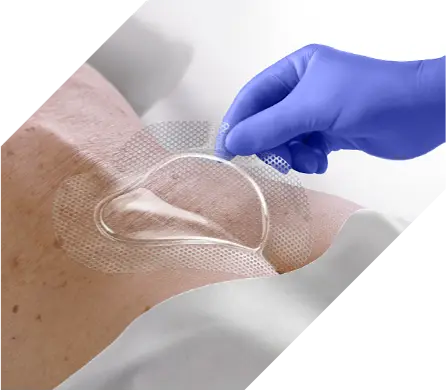
OptiView cuts the time and waste that comes with a lift-and-check approach to skin assessments. This innovative clear design allows caregivers to quickly and easily inspect, monitor and blanch skin with the dressing in place. The result is more time for care delivery.

Clear visibility extends wear time
Eliminating lift-and-check means fewer dressing changes, decreased nursing time and overall spend.
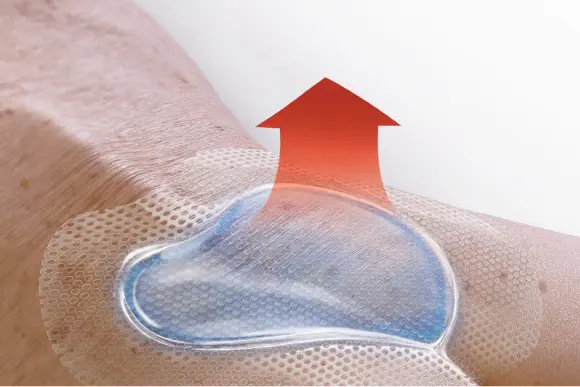
Manages microclimate with HydroCore technology
Pulls heat away from skin, effectively cooling skin temperature to reduce the risk of breakdown that results in pressure injuries (PIs).
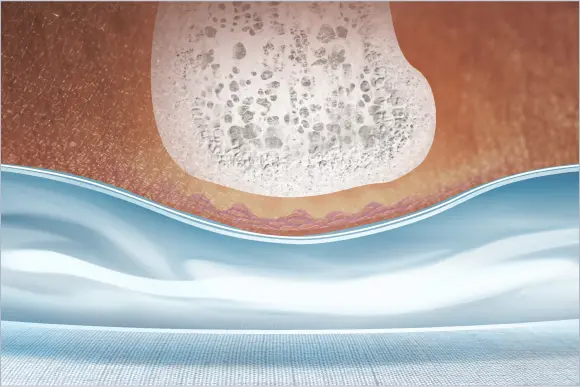
Redistributes pressure against bony areas
Performs like a foam dressing, reducing forces like pressure and shear across the dressing.

Helps prevent medical device-related pressure injuries (MDRPIs)
Improves visibility and manages pressure, shear and microclimate of the at-risk skin underneath medical devices.
OptiView outperforms leading foam dressings
Pressure and excess heat can lead to skin breakdown and increase the risk of pressure injury development. OptiView is shown to manage these risk factors better than leading competitors. Download the brochure to learn more about this transparent dressing.
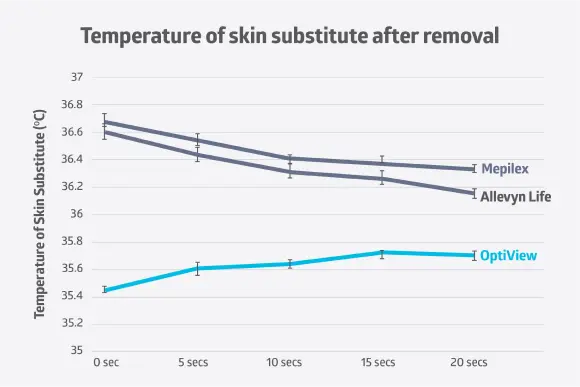
Helps keep skin up to 1.5°C cooler1
OptiView trapped less thermal heat on the skin’s surface, with an overall mean temperature that is 1.2° C to 1.5° C cooler than leading foam competitors.
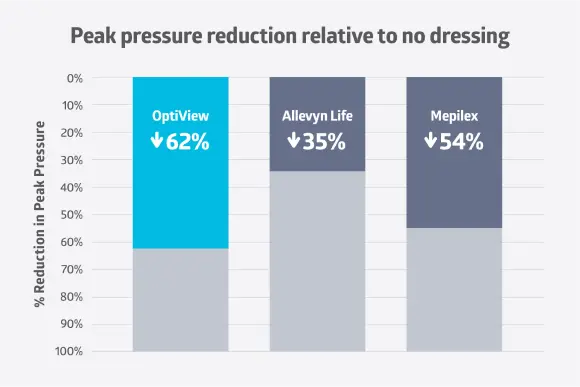
Reduces peak pressure by up to 27% more2
OptiView reduced peak pressure on vulnerable areas by 8 to 27% more than leading foam competitors.
Clinical trial results highlight better outcomes
A Connecticut hospital and Level 2 Trauma Center had the opportunity to experience this breakthrough dressing in their ICU. When used on 20 patients with intact skin on bony prominences, they found improved clinical and financial outcomes and more time for patient care.3
-Layla Nejati, WOCN at Danbury Hospital in Connecticut.

Get a clear view of at-risk skin with this proven dressing
Here’s how OptiView elevates your PI prevention protocol:
- Clear island: offers visibility of skin without the need to lift the dressing.
- HydroCore Technology: helps redistribute pressure, reduce shear and manage microclimate.
- Flexibility: up to 12 times more flexible than leading competitors, resulting in longer wear time.1
- Waterproof backing: helps protect underlying skin.
- Silicone face and border: aids in gentle removal.
Take the next step to improve skin assessments with OptiView
Simply complete this form and a Skin Health specialist will contact you soon to share more details about this innovative transparent dressing.
What caregivers are reading about PI prevention
References:
1. Study on file.
2.Study on file.
3.Study on file.


