How to help patients practice wound self-care at home


You play a critical role in your patients’ wound care, but these stressful times pose unprecedented challenges for all of us. As cases of COVID-19 continue to grow nationwide, non-essential businesses are closing to help control the spread. Recently, the Alliance of Wound Care Stakeholders released a statement in support of wound care as an “essential,” not elective, service,1 but many outpatient wound care centers have closed. At the same time, home healthcare nurses may no longer be able to visit people’s homes, and many wound care patients are being discharged sooner than usual from inpatient facilities.
For you and your patients, COVID-19 means a shift in care management: more at home, less in person. This does two things…
- Helps prevent wound care patients and their families from being exposed to the virus
- Frees up much-needed resources for the people suffering from COVID-19
Now more than ever, it’s important to empower your patients to help prevent and treat their wounds at home. They may feel nervous about both caring for their wound and about COVID-19. You can help. Here’s how.
Tips on how to best answer patient questions
Overall, it’s a stressful situation for everyone, so keep answers simple and feel free to use patient education resources to help further inform and build patients’ confidence.
A. Before they were discharged, your patients will have received at-home treatment instructions and the appropriate wound care products ordered by the physician. If they still have questions on which dressing to use for their particular wound, keep the information straightforward. Remind them that the dressing they use is based on the drainage and depth of their wound, and a little drainage is usually normal, so not to worry.
| Choosing the right wound dressing Based on the size and type of wound, this chart helps you guide patients’ wound-dressing choices – and how to use them. | ||
| Wound condition | Type of dressing and what to do | |
| Depth:
Superficial Moisture: Mostly dry Drainage: Little to none |
1. Apply a thin coat of a hydrogel. Hydrogel is a mix of glycerin and water that comes as a sticky gel and helps add moisture to a superficial wound. |
2. Cover with a bordered gauze or foam dressing. |
| Depth:
Deep wound (1/4-inch or greater) Moisture: Mostly dry Drainage: Minimal |
1. Gently fill or pack the wound with gauze moistened with hydrogel. |
2. Cover with a or foam dressing.  |
| Depth:
Superficial Moisture: Wet Drainage: Minimal |
Cover with foam dressing.
|
|
| Depth:
Deep wound (1/4-inch or greater) Moisture: Wet Drainage: Heavy |
1. Pack the wound with either an alginate or gelling fiber to help manage drainage and still keep the wound moist. |
2. Cover with a foam dressing.  |
A. This is a great question and probably on the minds of most patients. First, remind your patients to review any at-home treatment instructions they received from their healthcare provider. They can also read the directions on the wound care packaging or check the company’s website to see how long the dressing can remain on the skin before it needs to be changed. It might be anywhere from three to seven days, so here are two important points to make with patients:
- Watch for changes in drainage. It’s normal to see some drainage showing through a cover dressing, such as a bordered gauze or bordered foam, but if drainage is reaching the edge of the dressing or the dressing is discolored by drainage, then it’s time to change it, so the dressing doesn’t start to come off.
- Trust your own eyes. Remind patients that if they’re changing their dressing according to instructions – for example, every three days – but they’re seeing a lot of drainage every time, then it’s OK to change it more frequently, maybe every two days, until the drainage slows. Then, patients can return to their regular schedule.

A. It’s natural for patients and their loved ones to feel unsure and even worried about changing their wound dressing. Offer to help talk them through it with these simple steps.

- Before starting, wash hands thoroughly for at least 20 seconds.
- Gently remove the old dressing and discard it.
- Clean the wound with gauze, saline or a wound cleanser, whichever they’ve were instructed to use by their healthcare provider.
- Pat the wound dry.
- Place the new dressing on the wound.
- Secure or cover the wound with a cover dressing.
- Wash hands thoroughly for at least 20 seconds when finished.
Try to calm people’s fears by explaining there are more resources out there to help them feel more comfortable and confident caring for their wounds at home. For example, most wound care product manufacturers have charts, posters, videos and educational packaging that show you how to safely and successfully apply their wound dressings.

A. A lot of patients are frustrated by the slow healing process. Reassure them that their wound will get better with time, and there are things they can do to help. Encourage patients to consistently follow their recommended treatment. Remind them to eat healthy foods or take a liquid protein nutritional supplement – proper nutrition has been shown to be a key factor in wound healing.
A. It’s critical for people to know what to look for when it comes to wound infection. Remind patients or their loved ones to call their healthcare professional or, if necessary, 911, if they see any signs of infection.3

- Fever of above 101 that persists
- Foul-smelling green discharge from the wound
- Cloudy discharge from the wound
- Redness or increased swelling around the wound
- Hot skin around the wound
- Increased pain on the wound site
- Loss of normal movement of the wound area
A. While COVID-19 is still a risk, advise your patients to stay indoors to avoid contact with other community members. However, physical activity has been shown to improve blood flow and it may decrease healing time,4 so if their wound allows them to move around, you might suggest they walk safely around their house or up and down stairs. Just be sure they hold on to stair railings to keep from falling and move small rugs out of the way to avoid a tripping hazard.
A. If your patients are having a hard time with compression wraps, here’s an alternative to help reduce swelling and increase blood flow: Elevate the legs above the heart several times a day for 20 to 30 minutes each time.
A. Everyone’s concerned about the coronavirus, but the best advice you can offer your patients is to follow the Centers for Disease Control and Prevention’s guidelines on how to protect themselves: frequent hand washing, maintaining at least 6 feet from other people, and cleaning and disinfecting surfaces frequently. The CDC’s website, cdc.gov, offers the latest recommendations and news
Keep prevention top of mind with these two strategies:
1. Learn safety measures
While you’re helping your patients cope with clinic and facility closures, your hard work continues. Find out ways to control transmission of the virus through a series of important Medline University courses, such as “COVID-19: Airborne Transmission-Based Precautions in Post-Acute Care” and “COVID-19: Contact and Droplet Transmission-Based Precautions in the Acute Care Setting.”
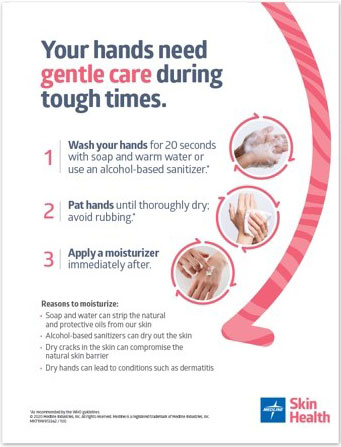
2. Share visual reminders
One of the best ways to prevent the spread of infection is by proper hand hygiene.
Download and share our hand hygiene poster to drive home proper hand-washing techniques and skin care.
Provide care and calm
During this stressful time, when there are so many questions on everyone’s minds, your simple, straightforward guidance can make a real difference. Empowering patients to confidently care for their wounds at home helps improve outcomes and keep people safe…while freeing up the much-needed resources to manage COVID-19.
References:
- https://aawconline.memberclicks.net/assets/docs/Alliance%20of%20Wound%20Care%20Stakeholders%20Statement%20on%20Wound%20Care%20as%20Essential….pdf (Accessed March 30, 2020)
- https://meddevod.wpdev.medline.com/product/Active-Liquid-Protein-Nutritional-Supplement/Oral-Nutritional-Supplements/Z05-PF10996?question=nutrition&index=P24&indexCount=24#mrkMore
- https://www.woundsource.com/blog/8-signs-wound-infection (Accessed March 30, 2020)
- https://jamanetwork.com/journals/jamadermatology/fullarticle/2705273 (Accessed March 30, 2020)
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/chronic-venous-insufficiency (Accessed March 30, 2020)