Know the challenges of wound healing
Most wounds progress through the stages of healing on their own, but some get stuck, often stalling in the inflammatory phase. When wounds don’t heal within 30 days, they’re considered chronic and need help to overcome barriers like biofilm.
Chronic wounds are estimated to affect between 3 to 6 million people and cost between $5 and $10 billion annually.1 With education, best practice guidance and a proven system of products, you can empower caregivers to help improve outcomes and cut costs.
90% of stalled wounds contain biofilm
Identify common chronic wounds to help guide treatment
When you’re able to recognize the most common wound types, it’s easier to choose the right products and protocols to promote healing. Consider the patient’s medical history, wound location, measurement and characteristics—shape, depth, drainage and pain levels—to more accurately identify the wound etiology.
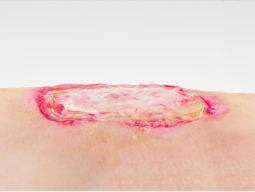
Venous leg ulcers (VLUs)
VLUs are shallow, moist wounds caused by skin breakdown from venous stasis. Compression and advanced wound care products help promote healing.

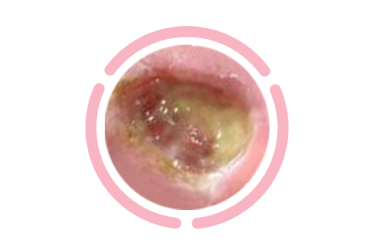
Pressure injuries (PIs)
These injuries—caused by pressure, friction and shear—require accurate assessment of the stage and proper turning and offloading.

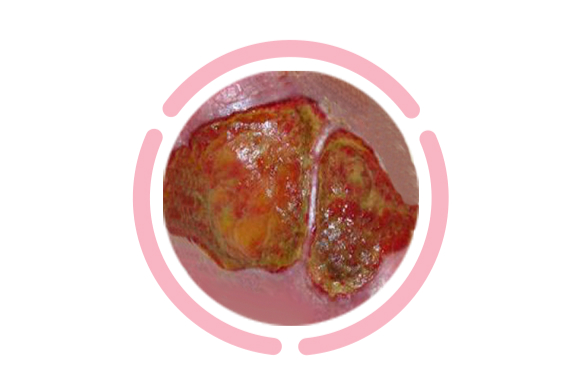
Diabetic foot ulcers (DFUs)
Poor blood flow, hyperglycemia and weight bearing can lead to DFUs, requiring pressure offloading and collaboration with a dietician.
Arterial wounds
Lack of blood flow and oxygen to legs results in dying tissue and open wounds. Immediate referral to a specicialist is a critical next step.
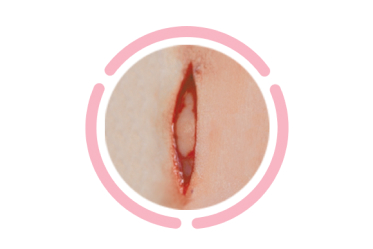
Surgical wounds
Infection can cause surgical incisions to reopen and stall healing. Advanced wound care products can help address this.
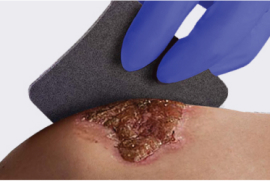
Optimize the wound bed to control infection
To heal infected wounds, start with the most intelligent dressing and then check the progress after two weeks. If the wound doesn’t improve, reassess and try something else. A slow-release iodine dressing and a wound cleanser with antimicrobial properties can help target bacteria, and a concentrated surfactant loosens and traps debris. Fight infection with a hydrating serum to promote a moist wound environment.
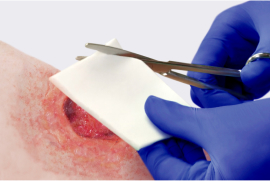
Close hard-to-heal wounds faster with advanced treatments
The most challenging chronic wounds call for advanced therapies. When standard methods aren’t enough, turn to innovative tools like collagen dressings, skin grafts, skin substitutes and negative pressure wound therapy. In fact, highly native collagen is highly effective in promoting wound closure as it preserves human collagen, which plays a key role in wound healing. Clinical nutrition can advance healing in stalled wounds and helps improve glycemic for diabetic patients.
Take the next step to elevate patient care
Our skin and wound care clinicians understand your challenges firsthand. Let us help you improve outcomes. Simply complete this form and a Skin Health specialist expert will reach out to discuss the best advanced wound care protocols for your facility.