How can EVS help reduce the spread of airborne diseases?
Controlling floating pathogens requires the addition of UV technology.
We’ve known for years that diseases such as pneumonia, tuberculosis and influenza can be spread through airborne microorganisms. In fact, among hospital patients with healthcare-associated infections (HAIs), healthcare-associated pneumonia is the leading cause of death and causes 22% of all HAIs.1 And mortality rates for nursing home residents diagnosed with pneumonia and requiring hospitalization range from 13% to 41%.2
Moreover, multi-drug resistant organisms (MRDOs) or “superbugs,” such as MRSA and C. difficile, are on the rise and can be transmitted via air.
Yet it wasn’t until the COVID-19 outbreak in March 2020 that airborne diseases took center stage. What exactly are these pathogens? Airborne diseases pass from one person to another when microorganisms—such as bacteria, fungi, or viruses—travel through the air in aerosolized particles.3
It’s clear that EVS workers face multiple challenges when it comes to keeping people safe from dangerous pathogens in the air.
Airborne diseases can spread through a direct or an indirect form of transmission, depending on the germ involved. The pathogens may enter the air in wet droplets, for example, when someone breathes or sneezes. There, they will be suspended in the air, and some droplets dry out, leaving microscopic particles. While suspended in the air, these particles can attach to or enter the bodies of people nearby.3
Even more troubling, these droplets can also land on surfaces in a patient or resident room. Everyone who enters a healthcare facility plays an important role in preventing the spread of airborne diseases, from wearing appropriate personal protective equipment (PPE) to practicing good hand hygiene. The bottom line is that environmental services (EVS) cleaning and disinfection protocols should include measures for addressing airborne pathogens.
“Air is an important piece. Think about the flu, for example. Flu droplets can spread the virus and the microorganisms can live on surfaces for a long period of time.”
Angela Zuick
Medline Director of Clinical Services
This article is one in a three-part “Clean Fast and Well” series covering EVS best practices for cleaning and disinfecting patient/resident rooms. (In the other two articles, we focus on hard surfaces and soft surfaces.)
Clearing the air
Engineers in healthcare facilities are primarily responsible for ensuring optimal air quality and cleanliness, for example, through appropriate air filtration and circulation systems, negative pressure rooms and HVAC systems. But it’s also important for EVS managers to take safety to the next level and make sure they’re taking steps to ensure a clean atmosphere.
Manual cleaning is your first line of defense in preventing the spread of infections. Adding technology is your second line of defense against airborne pathogens, and UV light is one of your main weapons. When UV light gets absorbed, the photons of light transfer their energy to and damage the chemical bonds of the genetic material. The virus is then unable to replicate or cause an infection.4
There are two main types of UV technology: mercury, which is highly effective on surfaces at closer distances; and pulsed xenon, which is ideal for whole room disinfection of common healthcare pathogens.
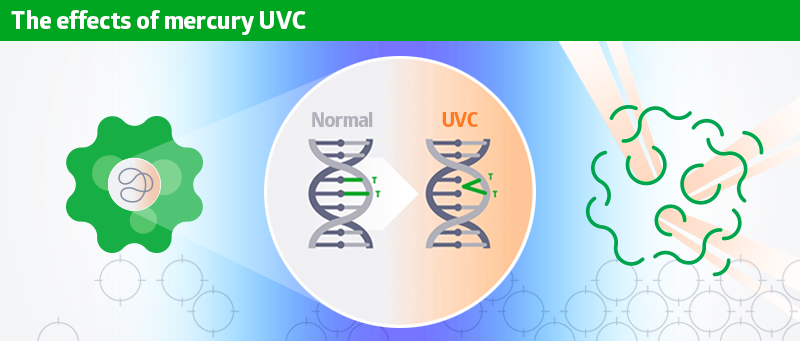
UVC light enters the cell and alters the DNA and RNA by creating thymine dimers, which either destroys the pathogen or prevents its reproduction.
A portable UV air disinfection device uses UVC energy to kill up to 99.9995% of airborne particulates. It’s safe to use while people are in the room, and it’s quiet while it continuously scrubs the air. Some devices use advanced HEPA and carbon filtration to remove allergens, odors and other volatile organic compound particulates.
This UV technology is especially useful when cleaning operating rooms between surgeries and isolation rooms between patients.
And let’s not forget the impact of odors on patient and resident satisfaction.
As pointed out by Angela Zuick, Medline Director of Clinical Services, “Your first perception upon entering a room in a hospital or nursing home is, ‘What is my room like? What does it smell like? Does it look like a sterile environment?’ People will not go to nearby healthcare facilities if they perceive them as being dirty.”
Lessons learned from COVID
During the pandemic, healthcare facilities have stepped up protocols to keep everyone in their facilities safe from airborne pathogens. CMM (Cleaning & Maintenance Management) highlights lessons learned to keep EVS workers safe as they clean and disinfect areas where these microorganisms can live:
- Review standard precautions and keep EVS workers informed—In some cases, EVS staff may not be able to properly assess the risk of exposure prior to patient interaction. The use of PPE can be effective only if the employee has a proper understanding of the pathogen likely to be encountered and the mode of transmission. Protocols should consider regular use of face protection.
- Plan for PPE and train staff how to use/wear it—Any PPE required for a surge in infections should be identified in advance to ensure there are no delays when it is ultimately required by EVS staff. And they should be regularly trained on how to use the equipment.
- Promote hand hygiene compliance—Healthcare facilities continuously monitor compliance of hand hygiene and should provide real-time feedback to EVS staff on proper technique.
- Mind the frequently touched surfaces—Good hand hygiene, proper glove use and adequate surface disinfection go hand in hand to reduce infection risk for patients and EVS staff.
- Don’t overlook the floors—There is mounting evidence that points to floor contamination with pathogenic organisms that can include MRSA and C. difficile. More research into proper floor maintenance is required.
- Use UV-C light as an added measure of safety, not the only measure—Surfaces should be cleaned and disinfected before boosting disinfection with UV-C light.5
Following these steps will help keep everyone safe and prevent transmission of airborne diseases.
Key takeaway
It’s natural to focus more on everyday surfaces when thinking about the cleaning and disinfection of rooms in healthcare facilities. But with the coronavirus outbreak, air cleanliness has become a key point of concern and EVS priority. While air quality is generally an engineering responsibility, EVS can use UV light technology to kill airborne pathogens and reduce the spread of HAIs.
References:
- Pulmonology Advisor. Hospital Acquired Pneumonia. Available at https://www.pulmonologyadvisor.com/home/decision-support-in-medicine/pulmonary-medicine/hospital-acquired-pneumonia/. Accessed Nov. 12, 2021.
- Stamm, Dustin; Katta, Shravan; and Stankewicz, Holly. Nursing Home Acquired Pneumonia. Stat Pearls Publishing. July 19, 2021. Available at https://www.ncbi.nlm.nih.gov/books/NBK537355/.
- Medical News Today. What to know about airborne diseases. Available at: Airborne diseases: Types, prevention, and symptoms (medicalnewstoday.com). Accessed November 14, 2021.
- The Conversation. Type of ultraviolet light most effective at killing coronavirus is also the safest to use around people. Available at: https://theconversation.com/type-of-ultraviolet-light-most-effective-at-killing-coronavirus-is-also-the-safest-to-use-around-people-169602. Accessed 11/16/21.
- Calabrese, Carol (2021). A Review of Cleanliness Protocols for Health Care EVS Workers. ccmonline.com, Aug. 26, 2021. Available at A Review of Cleanliness Protocols for Health Care EVS Workers | Cleaning & Maintenance Management (cmmonline.com).