Cleaning and disinfection of patient rooms: Surface pathogens
High-touch surfaces require the right protocols, processes and products.

A patient or resident in your facility has a tray table that has personal items, medical equipment or food on it at any given time. When do you clean the table? How often? With what product? Surface pathogens on that table can open the door to the spread of healthcare-associated infections (HAIs).
This article is one in a three-part “Clean Fast and Well” series covering EVS best practices for cleaning and disinfecting patient/resident rooms. (In the other two articles, we focus on soft surfaces and air.)
The toll it takes
Each year, approximately 1.7 million HAIs occur in US hospitals,1 and 1.3 million infections occur in long-term care facilities.2 The environment of care in your facility is one of three zones where an infection prevention strategy is crucial to keeping people safe.
With the pressure to clean and turn over rooms quickly, how can you ensure that patient/resident rooms are cleaned thoroughly and efficiently?
“The environment is the biggest piece, literally and figuratively,” says Angela Zuick, Medline Director of Clinical Services. “I think the challenge is we don’t adequately educate the EVS workers and help them realize that every action and stop they have in their process has these ripple effects.”
In fact, using tracer viruses, researchers found that contamination of just a single doorknob or tabletop results in the spread of viruses throughout office buildings, hotels and healthcare facilities. Within two to four hours, the virus could be detected on 40 to 60% of workers and visitors in the facilities and commonly touched objects.3
On the surface
The Centers for Disease Control and Prevention (CDC) has identified 17 high-touch surfaces4 in a care facility room. Not all rooms will have every surface on the CDC list, but it’s important to pay special attention to those in your facility that are on the list. The list includes:
- Bed rails/controls
- Tray table
- IV pole (grab area)
- Call box/button
- Telephone
- Bedside table handle
- Chair
- Room sink
- Room light switch
- Room inner doorknob
- Bathroom inner doorknob/plate
- Bathroom light switch
- Bathroom handrails by toilet
- Bathroom sink
- Toilet seat
- Toilet flush handle
- Toilet bedpan cleaner
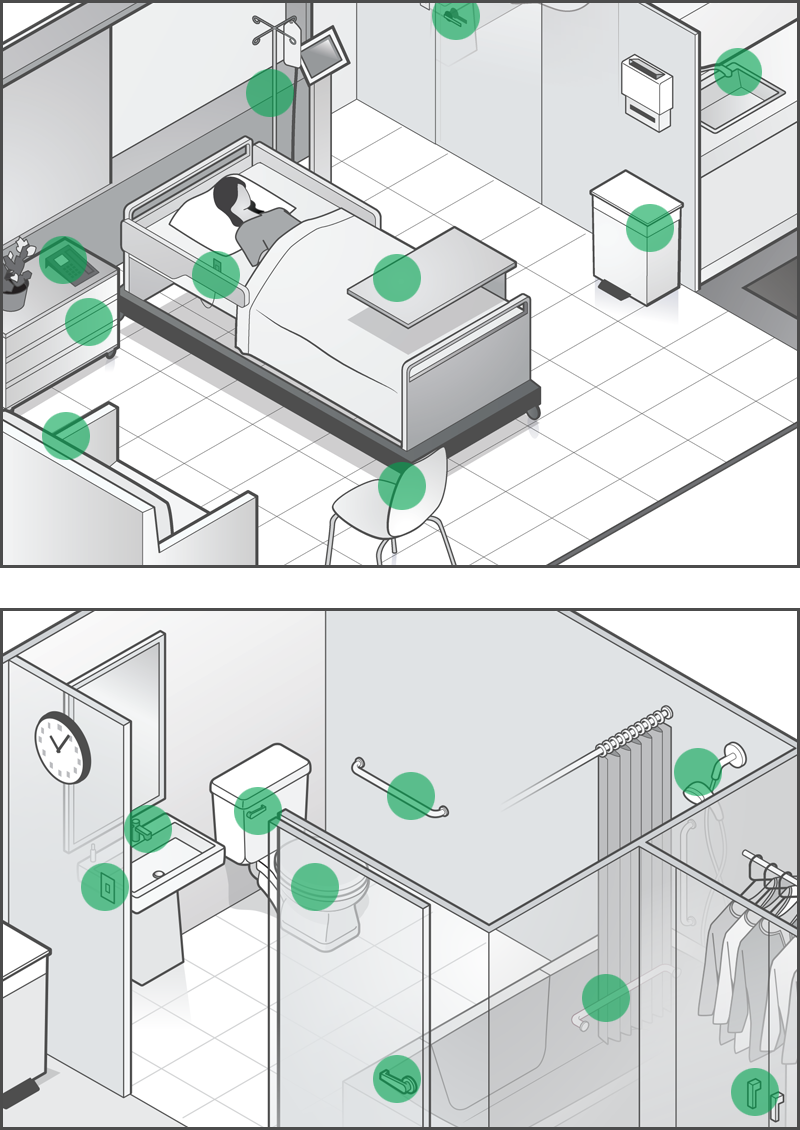
In long-term care facilities, showers and shower handrails are among the high-touch surfaces.
How many touches are a lot? For example, a bed rail can be touched upward of 256 times per day, while typical surface disinfection is done only once a day.5
“Bed rails are among the most frequently missed surfaces during cleaning. They’re often down and hidden by the linens,” says Zuick.
With so many surfaces out of sight, it can be challenging to keep all of them clean.
How do you do it?
An effective environmental cleaning program takes the right people, products and processes. Work with EVS staff to make sure they clean and disinfect hard surfaces—as well as the whole room—in the right sequence, with the right products, using the right methods every time:
1
Standardize your cleaning and disinfection protocols
Define the products, supplies, technologies, methods, responsibilities, sequence and frequency for cleaning hard surfaces.
Clearly define responsibilities for the cleaning and disinfection of noncritical equipment, shared medical equipment, and other electronics (for example ventilator surfaces, bar code scanners, point-of-care devices, mobile workstations, mobile phones and tablets).6
When you determine the sequence of cleaning, make sure all surfaces are addressed and cleaned in an order that avoids cross-contamination. For example, outline where to start in the room and which cloth/mop/wipe and product should be used for each surface. And clearly delineate contact times (how long they need to “sit”) for products to ensure that pathogens are killed.
5 months
C. diff can live on an unclean surface for up to 5 months.7
Keep in mind that processes should be modified accordingly for turning over a private room, turning over a semi-private room, everyday cleaning of a private room and everyday cleaning of a semi-private room. As appropriate, use technologies that help between thorough cleanings. For example, employ devices that help to disinfect surfaces while people are out of the room, such as UV light systems.
2
Educate and train EVS staff to ensure they understand their roles and responsibilities
Teach staff your EVS policies, ensuring that they understand and value policies and are well positioned to follow them. They should also learn the basic concepts of pathogen transmission. Everyone should recognize the impact of their work on infection control and the safety of all people in the facility.
Further, staff should understand and follow protocols for protecting themselves while working, including proper use of personal protective equipment (PPE) and safe use of chemicals and cleaning technologies.8
Make sure to re-educate and re-train—especially as protocols are modified, technologies evolve and new products are introduced.
“The environment is the biggest piece, literally and figuratively. I think the challenge is we don’t adequately educate the EVS workers and help them realize that every action and stop they have in their process has these ripple effects.”
Angela Zuick
Medline Director of Clinical Services
3
Monitor and evaluate effectiveness and adherence to protocols, then take appropriate steps
Make sure to include: who should do the monitoring, what type of monitoring will be used (for example, direct observation, fluorescent gel or ATP), how frequently the monitoring will occur, how monitoring data will be validated, which rooms will be monitored and which surfaces will be assessed.9
By following these steps, you’ll help your facility reduce HAIs and increase the safety of all who enter.
Key takeaway
The environmental services team plays an important role in preventing HAIs in acute- and post-acute care facilities. But pressure to turn over rooms quickly, a lack of formal protocols, unclear responsibilities and limited resources can make it challenging to ensure the appropriate cleaning and disinfection of a patient or resident room every time. By establishing clear protocols and processes, delineating responsibilities, educating and training staff, and using the right products and supplies the right way, you can help keep everyone safe in your facility.
References:
- Klevens, RM, et al. Public Health Reports. 2007; 122:160-166. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1820440/
- Nursing Homes and Assisted Living (Long-term Care Facilities [LTCFs]). Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/longtermcare/index.html. Accessed July 11, 2019.
- American Society for Microbiology. How quickly viruses can contaminate buildings—from just a single doorknob. ScienceDaily, September 8, 2014. Available at How quickly viruses can contaminate buildings—from just a single doorknob—ScienceDaily.
- CDC Environmental Checklist for Monitoring Terminal Cleaning. Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/hai/pdfs/toolkits/environmental-cleaning-checklist-10-6-2010.pdf. Accessed November 4, 2021.
- Calabrese, Carol (2021). A Review of Cleanliness Protocols for Health Care EVS Workers. ccmonline.com, Aug. 26, 2021. Available at A Review of Cleanliness Protocols for Health Care EVS Workers | Cleaning & Maintenance Management (cmmonline.com). Accessed November. 1, 2021.
- Reduce Risk from Surfaces. Centers for Disease Control and Infection. Available at: Reduce Risk from Surfaces | HAI | CDC. Accessed November 2, 2021.
- Claro, Tania; Daniels, Stephen; and Humphreys, Hilary. Detecting Clostridium difficile Spores from Inanimate Surfaces of the Hospital Environment: Which Method is Best? J Clin Microbiol. 2014 Sep; 52(9): 3426-3428. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4313175/
- Reduce Risk from Surfaces. Centers for Disease Control and Infection. Available at: Reduce Risk from Surfaces | HAI | CDC. Accessed November 2, 2021.
- Ibid