Target zero harm with a 3-zone infection prevention strategy
Learn how to address all risk areas to improve patient and resident safety.

What does it take for pathogens to quickly spread and eventually cause a healthcare-associated infection (HAI)? Germs or pathogens need a place to live, a susceptible person and a way to be transmitted.
In a typical hospital environment, 1 in 25 patients has at least one HAI.1 The Centers for Disease Control and Prevention (CDC) and Centers for Medicare & Medicaid Services (CMS) call these infections “never events,” meaning that the practice of evidence-based care should prevent them. However, the reality is challenging and complex.
1 in 25 patients
in US hospitals has at least one HAI.1
It can be overwhelming to continuously prevent HAIs, considering the number of ill and medically compromised people in acute care and long-term care settings. But the everyday routines and practices of healthcare workers determine whether or not pathogens spread. Everyone plays a role.
Use a 3-zone strategy to target zero harm
For healthcare facilities, doing better means finding ways to get closer to achieving “zero harm,” a term that refers to the concept that no patients will be harmed by their interactions with a healthcare system. The Joint Commission says, “Zero harm doesn’t mean zero mistakes.” It does mean:
- Developing systems and processes that reduce the likelihood of mistake
- Creating a safety culture from leaders to frontline workers
- Championing procedures that catch errors or unsafe conditions before they cause harm
Where do you start? Focus on the three key zones of risk where infection is transmitted:
- Environment of care
- Human-to-human transmission
- Clinical practice
This 3-zone strategy breaks down infection prevention into smaller, more manageable parts. The key to success? Making sure everyone at every level is involved, understands the 3-zone strategy and practices infection prevention, consistently.

“The zones are really a breakthrough,” says Angela Newman, Medline Senior Director of Clinical Services. “They help organizations look at every aspect of infection and ask, ‘How can we improve best practices? What training and education do we need to close gaps? Which products will best support our people and keep everyone safe?’”
So often, infection prevention is thought of in silos: environmental services (EVS) here, clinicians there and materials management elsewhere. But the three zones interconnect and cross over all the time.
“In one interaction with a patient, you’re very likely to touch all three zones,” says Donna Matocha, DNP, Medline Manager of Clinical Resources–Critical Care. “Let’s say, I’m a clinician putting in a central line at the bedside. If the EVS worker didn’t wipe down the bed rail and I put my gloved hand on it and then touch the patient, all three zones had a failure. The zones are always impacting each other.”
In one interaction with a patient, you’re very likely to touch all three zones.

Donna Matocha, DNP
Medline Manager of Clinical Resources–Critical Care
“To improve infection prevention metrics, you have to empower and engage everyone,” says Matocha. “The key is to inspire everyone to take ownership and help them understand the vital role they play in preventing HAIs across the organization. Shared accountability is key.”
The 3 zones of infection prevention

Zone 1: Environment of care—keep it clean
A patient or resident room and bathroom—or anywhere in the environment of care—provide many places for germs to live. From faucets to floors, bed linens to bed rails, and monitors to medical devices, pathogens are lurking and ready to spread.
72% of hospital floor sites
tested positive for C. difficile 6
EVS teams play a critical role in cleaning and disinfecting hard surfaces, soft surfaces and air. Yet, EVS managers and staff face challenges such as a lack of clear-cut guidelines for products to use to clean surfaces. This issue can be resolved by using an evidence-based cleaning and disinfection program.
As an extra layer of protection, UV light technology can be added to complement manual cleaning processes.
“These programs can provide EVS workers training and education on evidence-based products that can help prevent the spread of germs,” says Newman.

Zone 2: Human-to-human transmission—pair hand hygiene and PPE
Coughs, sneezes, touch. In the human-to-human transmission zone of a healthcare setting, unchecked pathogens can easily cause infection through hand, face and bodily contact. Personal protective equipment (PPE)—such as face masks, air-purifying respirators, gowns and gloves—and hand hygiene products and practices protect patients, residents, family, visitors and staff against germs.
“The number one way to help fight infection is simple: wash your hands,” says Newman. “In fact, hand hygiene is fundamental to all three zones. Everyone coming into the hospital—family members, delivery people and staff—has to practice proper hand hygiene to prevent germ transmission.”
Only 40% of healthcare workers
adequately comply with hand hygiene practices5
Many device-related infections happen because people don’t practice hand hygiene or use PPE properly. And visitors and family often don’t realize their hands could contaminate their loved ones’ devices. Being vigilant about hand hygiene and the use of PPE can help minimize transmission.
And let’s assume all patients and residents are carrying pathogens that can be spread. You can use universal decolonization to keep them safe. A total body approach focuses on nose, mouth and skin.

Zone 3: Clinical practice—eliminate CLABSI and CAUTI
In the clinical practice zone, catheters cause some of the most common HAIs. Central venous catheters (CVCs) and indwelling urinary catheters (IUCs) are access points and breeding grounds for germs that can lead to central line-associated blood stream infections (CLABSIs) and catheter-associated urinary tract infections (CAUTIs).
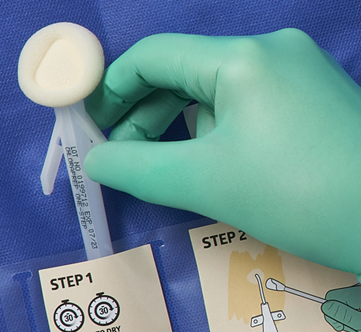
Clinicians insert, access and maintain CVCs and IUCs multiple times a day. The way to prevent CLABSI and CAUTI is to standardize care. Having a system of products, such as clinical kits for central line insertion and maintenance, helps clinicians reduce variation and error—and minimize risk of infection.
“Clinical kits, which bundle everything a nurse would need in the right sequence, make it easier for them to do the right thing no matter how busy their floor might be,” says Newman.
30,000+ CLABSIs
occur annually in hospitals and
nursing homes,2 with a
patient mortality rate of 12-25%3
75% of all UTIs
are associated with an indwelling urinary catheter4
Before using an IUC insertion kit, determine if an IUC is necessary. The best way to prevent CAUTI is to avoid using an IUC and instead use external catheters when possible.
Matocha says bundles should be well-engineered from a human factor standpoint.
“If you use the components in sequence, you should be able to do the procedure correctly whether you’re a resident or experienced nurse. That’s a major step toward zero harm,” she adds.

Build a culture of shared accountability
Infection prevention ultimately should belong to everyone in your organization. It takes a culture shift to make it happen. To help people feel more empowered and become more engaged in shifting culture, consider taking the following steps:
- Identify a champion in each unit, including EVS, the lab, ancillary units and others across the continuum
- Include the EVS director in cross-functional weekly rounds and monthly meetings, and take steps to build a collaborative relationship with them
- Celebrate small successes together to build pride, ownership and accountability

“At the end of the day, everyone wants that magic zero number,” Newman concludes. “It’s still a long journey to get there, but the good news is today there are more resources and evidence-based solutions to help you and your organization along the way.”
Key takeaway
Preventing HAIs is an ongoing challenge. You can cover the full perimeter of risk by using a 3-zone strategy that emphasizes people, process and products. This approach helps you empower teams to work together and create a culture of shared accountability and safety.
References:
- Magill, S.S., et al. (2014, March 27). Multistate Point-Prevalence Survey of Health Care-Associated Infections. The New England Journal of Medicine, 368(13), 1198-1208. https://www.nejm.org/doi/pdf/10.1056/NEJMoa1306801
- National Healthcare Safety Network. (2022, January). Bloodstream Infection Event (Central Line-Associated Bloodstream Infection and Non-central Line Associated Bloodstream Infection). https://www.cdc.gov/nhsn/pdfs/pscmanual/4psc_clabscurrent.pdf
- Woodward, B., and Umberger, R. (2016, October-December). Review of Best Practices for CLABSI Prevention and the Impact of Recent Legislation on CLABSI Reporting. Sage Open, 1-7. https://journals.sagepub.com/doi/pdf/10.1177/2158244016677747
- Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of Healthcare Quality Promotion (DHQP) Page last reviewed: October 16, 2015. https://www.cdc.gov/hai/ca_uti/uti.html
- Centers for Disease Control and Prevention. (2002, October 25). Morbidity and Mortality Weekly Report: Guideline for Hand Hygiene in Health-Care Setting, 51(RR-16), 22. RR5116-Front Cover.p65 (cdc.gov)
- Desphande, A. et al. (2017, March 1). Are Hospital Floors an Underappreciated Reservoir for Transmission of Clostridium Difficile and Methicillin-Resistant Staphylococcus Aureus? American Journal of Infection Control, 45(3):336-338. https://pubmed.ncbi.nlm.nih.gov/28254251/




