Moisture-associated dermatitis vs. pressure ulcer education
Here’s your guide to help identify IAD so you can prevent and treat it properly.
Incontinence associated dermatitis (IAD) is a type of moisture-associated skin damage. It’s a common problem in healthcare facilities. Studies show prevalence rates in hospitals are about 7.5 percent and in nursing homes as high as 30 percent.
7.5%
Rate of IAD in hospitals1,2
30%
Rate of IAD in nursing homes1,2
The problem is, IAD isn’t always identified properly; it’s frequently confused with pressure injuries. “In my practice, I find approximately 45 percent of incontinence associated dermatitis presentations are mislabeled as stage 2 pressure injuries,” says Catherine Milne, MSN, APRN, CWOCN, BC-ANP, co-owner of Connecticut Clinical Nursing Associates and a Medline consultant.
“The interventions that we do to prevent PI are different than the interventions that we should be doing to prevent or treat IAD,” says Barbara Bates-Jensen, PhD, RN, WOCN, FAAN, Professor of Nursing and Medicine, University of California, and Medline consultant in a Medline Skin Health webinar. “If we’re misdiagnosing IAD as a pressure injury, we’re likely not intervening correctly for the problem.”
Understanding the differences between IAD and pressure injuries is an important step toward using resources efficiently and providing the best care for your patients. That’s why we created this guide that you can download to share with nursing staff as an at-a-glance educational resource.
Why knowing how to spot IAD is important:
- Proper assessment of patient skin conditions leads to the right treatment and better outcomes.
- Accurate data helps reveal the problem, which can inform quality initiatives to address it on a larger scale.
- Healthcare facilities avoid unnecessary regulatory fines now related to facility-acquired pressure injuries.
- Potential nursing home residents get a better picture of the quality of care at a facility.
What is IAD?
Incontinence associated dermatitis is inflammation of the outer layers of the skin in response to external surface irritants like stool or urine.
What is a pressure injury?
A pressure injury is also inflammation of outer as well as underlying layers of the skin, in response to forces of a person’s bodyweight or external forces such as from a medical device.
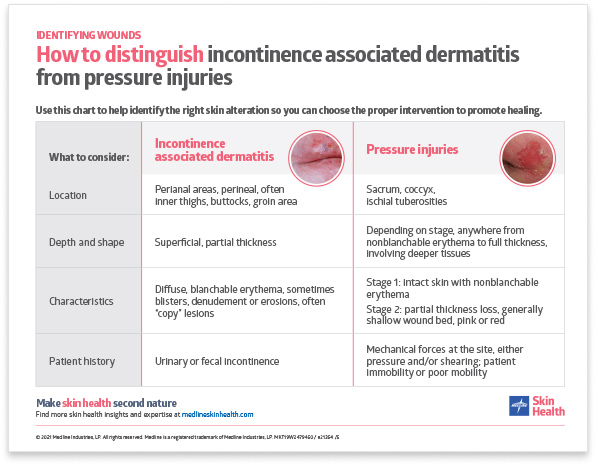
Four ways to distinguish IAD and PI
It’s helpful to have some simple ways to recognize the differences between incontinence associated dermatitis and pressure injuries. Dr. Bates-Jensen boils it down to four factors: location, depth, characteristics and history.
1 | Location
Incontinence associated dermatitis: Skin damage is focused around perianal and perineal areas, as well as often inner thighs, buttocks and groin.
Pressure injury: Pressure injuries often occur over bony prominences or under a medical device. They’re typically seen on the sacrum, the coccyx and the ischial tuberosities.
2 | Depth and shape
IAD: You’ll typically see multiple, superficial open lesions, spread over a large area, with partial thickness loss of skin. They may include blisters, denudement of the skin or erosions.
PI: Although depth and shape can vary, look for round or oval wounds that are deeper and may also include undermining or tunneling.

3 | Characteristics
IAD: Diffuse, blanchable erythema is often seen with copy lesions or blisters where there’s denuded or eroded areas. Copy lesions happen when moisture gets trapped on one side of the buttocks, then the other side aligns with it, spreading the moisture to both sides. Edges are usually irregular, with damaged and intact skin blended. You may also see fungal infection or candidiasis, which will show up as a rash. Patients may complain of pain, itching and burning.
PI: IAD is most commonly confused with stage 2 pressure injuries, which show up as a partial thickness loss of skin that involves the outer layers of tissue. Learn more about pressure injury stages with our visual explanation guide.
4 | History
IAD: Seems obvious, but remember to check to see whether your patient has a history of urinary or fecal incontinence, because that’s a telltale sign that the skin condition is IAD.
PI: Often, a patient with a pressure injury is often immobile or has poor mobility. You may also see friction and shearing at the site of the skin damage.
Treating incontinence associated dermatitis
“When you see redness, the opportunity for prevention has been lost,” Milne notes. So what do you do?
“First, try to enlist a knowledgeable colleague to determine what is truly causing the incontinence and, of course, protect the skin from further breakdown,” Milne advises.
Here are some options to help care for patients with IAD:
- External female collection device or condom catheter.
- Body-worn absorbent product such as a brief.
- Gentle pH-balanced skin care for cleansing, moisturizing and applying a protective barrier.
- Cyanoacrylate liquid skin protectant, which can be less painful and longer-lasting than pastes.
Key takeaway
“Without proper identification and prevention of IAD, your patients are at higher risk for skin breakdown and pressure injuries,” Milne stresses. Understanding the difference between incontinence associated dermatitis and a pressure injury can help prevent more serious skin breakdown. This guide can help empower your team to help make skin health second nature.
Explore more content about moisture-associated skin damage and pressure injuries:
Incontinence: Highlight the problem to lower risk of IAD and pressure injuries
Watch the webinar: Incontinence associated dermatitis: challenges and innovations in care
What more can you do to fight MASD?
Build staff knowledge and confidence with CE courses focused on skin and wound care best practices
Pressure injury staging is as easy as Apple P.I.E. (pressure injury explanation)
References:
- Campbell, J., Cook, J. L., Doubrovsky, A., Vann, A., McNamara, G., & Coyer, F. (2019). Exploring Incontinence-Associated Dermatitis in a Single Center Intensive Care Unit. Journal of Wound, Ostomy & Continence Nursing, 46(5), 401–407. Available at https://doi.org/10.1097/won.0000000000000571
- Kayser, S. A., Phipps, L., VanGilder, C. A., & Lachenbruch, C. (2019). Examining Prevalence and Risk Factors of Incontinence-Associated Dermatitis Using the International Pressure Ulcer Prevalence Survey. Journal of Wound, Ostomy & Continence Nursing, 46(4), 285–290. Available at https://doi.org/10.1097/won.0000000000000548