Know the risks of excessive skin moisture
Healthy skin requires some moisture, but too much can compromise the skin’s natural barrier, leading to negative outcomes, including:
- Fungal or bacterial infection because skin is more permeable
- Increased friction and shear, resulting in potential pressure injury formation
- Pain, burning and severe itching
- Delayed wound healing
- Embarrassing odor, impacting patient’s quality of life
It’s important to support caregivers with education combined with a proven system of products to help prevent and manage MASD.
What is MASD?
MASD is defined as an erosion or inflammation of the skin caused by long-term exposure to moisture.
Recognize the 4 types of MASD to deliver proper treatment
Moisture-associated skin damage is typically categorized by the source of the moisture. When caregivers know how to identify each type of MASD, they’re better prepared to properly manage it and prevent further skin breakdown.
Intertriginous dermatitis or intertrigo (ITD)
Skin breakdown from sweat trapped in skinfolds, leading to skin-on-skin friction.
Incontinence- associated dermatitis (IAD)
Damage from urine or stool around the groin, buttocks, inner thigh, perianal and perineal.
Periwound
moisture-associated dermatitis
Tissue at the edge of a wound that’s damaged due to caustic exudate.
Peristomal
moisture-associated dermatitis
Inflammation and erosion of the skin caused by discharge from an ostomy.
Maintain daily skin routines to fight skin breakdown
Managing moisture-associated skin damage starts with consistent daily skin care. In its consensus report on MASD, Wounds International recommends choosing a pH-balanced cleanser, washing with lukewarm water and soft cloths, and avoiding soap and water. When treating incontinence, Remedy Phytoplex Hydrating No-Rinse Foam Cleanser delivers a foaming wash with no rinsing required. Be sure to cleanse at least once a day and after each incontinent episode.

Create a robust barrier to guard skin
Protocols that prevent moisture from sitting on the skin for long periods might include reducing incontinent episodes with structured bathroom visits. But some comorbidities or immobility may make it difficult for caregivers to avoid moisture buildup. That’s why it’s important to help prevent skin breakdown with proven products, including drypads and long-lasting skin barriers such as Marathon. Shown to be five times thicker than other barriers, Marathon also helps protect against periwound and peristomal moisture damage.

Protect vulnerable skinfolds from bacteria
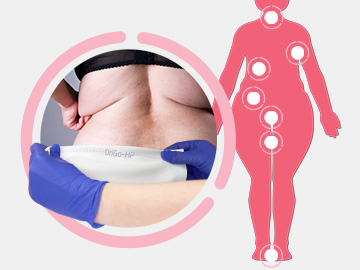
Warmth and moisture on the skin can contribute to skin damage, especially for bariatric patients whose vulnerable skinfolds can get irritated and lead to ITD. Instead of using powders, gauze and towels that may increase friction, Wounds International recommends moisture-wicking fabrics. DriGo-HP Antibacterial Wicking Sheet uses specially formulated hydrogen peroxide to help manage trapped moisture, minimize skin-on-skin friction and reduce odor.

Take the next step to standardizing moisture management
Simply complete this form and a Medline Skin Health specialist will contact you soon to discuss the best protocols to reduce moisture-associated skin damage at your facility.