Biofilm treatment protocol for managing chronic wounds
What experts recommend for breaking down the biofilms that stall wounds.

When you help a chronic wound turn the corner to healing, it’s a well-deserved victory. But wounds can be stubborn, and wound care experts are now realizing that one of the biggest barriers to healing is biofilm formation.
Stage 1
Free-floating or planktonic bacteria attach to a surface in a moist environment and begin to produce a protective layer referred to as the extracellular polymeric substance (EPS).
Stage 2
EPS holds the biofilm together and allows it to develop a complex community of sometimes up to hundreds of types of bacteria.
Stage 3
Groups of cells detach and form new attachments, leading to continued growth of the biofilm.
For wound healing, biofilm poses several challenges:
- Stimulates inflammation
- Elevates levels of proteases to harmful levels
- Increases exudate and fibrin slough
“Managing biofilm requires aggressive action. No half measures will be successful.“

Dr. Randall Wolcott
leading wound care expert and Medline consultant
Clinicians know that biofilm treatment is difficult. These communities of bacteria have been around for billions of years, having survived catastrophic events, according to Dr. Randall Wolcott, a leading wound care expert and Medline consultant.
In his webinar on chronic wounds and biofilm, he points out, “You don’t live 4 billion years by being lucky.” He adds, “Managing biofilm requires aggressive action. No half measures will be successful.”
Debridement
As part of the first step of wound healing, a surfactant-based wound care gel helps by proving gentle debridement. It removes barriers to healing, such as necrotic tissue and slough. Its distinctive formulation creates a gentle rinsing effect on a molecular level. The result is a softening and loosening of debris on the wound bed.
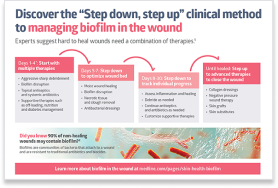
Elevate your biofilm protocol with this proven approach
According to wound care experts such as Dr. Wolcott, a “Step down, step up” approach is best for treating biofilms.1 Breaking down the biofilms that delay healing starts with debridement.
Combination therapies
While debridement is essential to reducing biofilm, it doesn’t get rid of it completely. After seeing improvement in a wound, it’s time to step down by customizing a combination of healing therapies that may include an antibacterial dressing. A combination of therapies can help optimize the wound bed and speed along the healing process.
Keep checking in
Throughout the process of healing, be sure to regularly reassess each individual wound to make sure your plan is still working. Each patient is different and may have varied colonization and comorbidities. You may need to step back up and down multiple times. Your persistence and efforts with hard-to-heal wounds can help keep biofilm at bay and allow the wound to heal.
When it comes to disrupting the biofilm that delays healing, you need proven interventions. We’ve gathered the data behind two reliable products that can help you implement the step down, step up biofilm protocol and advance wound healing for your patients.
Proven science4
In an ex vivo study on pig skin, researchers compared bacterial biofilm levels using two different methods:
- A surfactant-based wound gel
- Traditional wiping with saline-moistened gauze
After a three-day regimen of either surfactant or gauze, total bacteria in the surfactant-treated explants steadily decreased, with no detectable bacteria on day three. The wiping-only control bacteria counts initially decreased, but by day three were back to original counts.
IoPlex® Iodophor Foam Dressing
IoPlex is a hydrophilic absorbent foam dressing complexed with slow-release iodine for biofilm management. There’s convincing data on the effectiveness of this iodine dressing, which is why clinicians use it after debridement as part of the step down approach. It’s been shown to manage biofilm in-vitro and reduce bacterial burden within the wound dressing.1 Its unique controlled-release system allows for regulated and sustained infection management through the slow release of iodine within the wound dressing. Experience IoPlex for yourself.
Key takeaway
Biofilm presents arguably the greatest barrier to healing challenging wounds. It’s important to understand the mechanisms of biofilm in order to manage it and help those difficult wounds heal. Using the right treatment protocol, including combination therapies with the right biofilm disruptors will help you advance healing.
References:
- Attinger, C., & Wolcott, R. Clinically Addressing Biofilm in Chronic Wounds. Advances in wound care. 2012;1(3), 127–132. doi:10.1089/wound.2011.0333
- Schultz G, Bjarnsholt T, James GA, et al. Consensus guidelines for the identification and treatment of biofilms in chronic nonhealing wounds. Wound Repair and Regeneration. 2017;25(5):744-757. doi:10.1111/wrr.12590
- Yang Q, Larcose C, Porta AD, Della Porta AC, Schultz GS, Gibson DJ. A surfactant-based wound dressing can reduce bacterial biofilms in a porcine skin explant model. International Wound Journal. 2017;14(2):408-413
- Data on file.