Medical mattresses: Would yours pass inspection?
Replace pressure redistribution mattresses to deliver better outcomes.

Topics covered:
DETECTING DAMAGE | ACTION PLAN | PRESSURE INJURY PREVENTION |INFECTION CONTROL
From emergency department to hospital room to long-term care facility, in every care setting, people encounter a medical mattress, often more than one in a single day. Mattresses can help support your clinical goals by providing proper pressure redistribution and infection prevention. But if your mattresses are damaged or worn, they could be doing more harm than good.
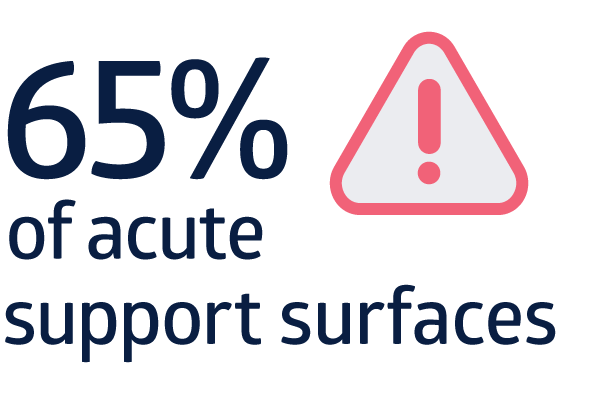
needed immediate replacement1

are compromised within 4 years2
In a Medline assessment of over 5,000 acute care support surfaces, 65% of them required immediate replacement.1 An assessment of more than 33,000 nursing home surfaces showed that 50% are compromised within 4 years. And mattresses that needed immediate replacement were already an average of almost 9 years old.2 Download the studies
Read on to discover why medical mattress assessments are an important part of overall patient and resident skin health. Learn how to identify mattresses that should be replaced and establish effective mattress management.
Know when to replace or upgrade mattresses
The American Hospital Association recommends replacing mattresses every 5 years.5 However, this routine is rarely enforced, and clinicians often overlook the wear and tear on mattresses. The 5-year recommendation should serve only as a guide. The lifespan of any mattress depends on usage and factors that can lead to the failure of a support surface.
Even though a manufacturer may list a warranty for manufacturing defects of 10 years, some clinicians mistake this warranty for an expected life expectancy. In fact, many factors can mean that the mattress won’t last those 10 years. Our mattress assessment study concluded, “Most support surfaces analyzed in the study are unsuitable for patient care.”
That’s why it’s important for clinicians at every point of care to know what to look for when it comes to detecting failing mattresses. NPIAP emphasizes, “Examine the functionality of the support surface on every encounter.”

8 warning signs of possible mattress failure:
1. Wearing or thinning of mattress cover
2. Tears
3. Holes
4. Stains
5. Torn zippers
6. Fluid in the mattress
7. Compromised internal structure
8. Compressed
Develop a mattress action plan and replacement protocols
Meador says facilities should be inspecting every mattress on an annual basis. Indications of mattress failure signal it’s time to take action. The problem is, Meador says, “A lot of facilities think someone will let them know if a mattress has a failure, but the truth is, it becomes a question of ‘Whose job is it?’”
Clinicians might not have time for mattress inspection built into their busy day. A knowledgeable vendor partner can work with you to set up and implement a comprehensive mattress assessment. They’ll look for signs of mattress failure and will tag every mattress with a green, yellow or red tag to indicate it’s OK, at risk or ready for immediate replacement.
Be sure you’re able to work together to inspect all brands of mattresses in your facility. Being proactive can help prevent mattress failure from contributing to skin breakdown or infection.
FDA tips to help identify at-risk mattresses
The FDA has developed some simple guidelines to help keep patients safe from contaminated mattresses. They cover the following information:
Develop a mattress inspection plan
Check the manufacturer’s guidelines for the expected lifetime of your hospital mattresses and mattress covers and follow their recommendations. Also consider factors such as mattress usage and patient acuity. Individuals might be on mattresses for prolonged periods, causing the mattress to become compressed sooner than expected.
Conduct mattress inspections
Schedule regular mattress and mattress cover checks for any visible signs of damage or wear. Discard and replace Immediately replace damaged, worn or visibly stained mattresses and covers to reduce the risk of infection.
Maintain inventory
Undamaged mattress covers should be routinely cleaned and disinfected according to the manufacturer’s guidelines. Be sure to use proper cleaning products and methods. Harsh chemicals in some cleaners can break down mattress cover material. Watch for staining on mattresses; their presence may lead to more vigorous and frequent cleaning, which can further damage the cover material.
Why do medical mattresses matter to skin health?
There are two key reasons to know the state of your mattresses and when it’s time to replace them: pressure injury prevention and infection prevention.
Support surfaces can mitigate pressure injury risk by redistributing pressure, managing friction and shear, managing the microclimate.
Mattresses can help with pressure injury prevention
“A mattress is a piece of the pressure injury prevention puzzle,” says Anita Meador, Medline Senior Manager, Clinical Resources. In fact, the National Pressure Injury Advisory Panel (NPIAP) devotes an entire section to support surfaces in their clinical guidelines, underscoring their significance.
“Support surfaces can mitigate pressure injury risk by redistributing pressure, managing friction and shear, managing the microclimate,” the NPIAP guidelines state. Depending on specific mattresses your facility chooses, they may provide different levels of protection. But no matter your mattress selection, the NPIAP warns that a hard mattress can contribute to the formation of pressure injuries.3
The NPIAP also explains that an appropriate mattress will do two important things when it comes to preventing pressure injury formation:3
- Redistribute an individual’s weight over a larger area and conform to the shape of their body
- More evenly distribute pressure to avoid concentrating pressure over bony prominences where pressure injuries typically develop
Bottom line, NPIAP says: “Support surfaces play a significant role in an individualized comprehensive management plan for pressure injury prevention and treatment.”3
Mattresses are part of infection control
Your facility is already focused on infection prevention, and mattresses should be part of that. “Mattresses that are faulty are a portal for infection,” Meador says. “So you need to make sure covers are cleaned properly and replaced when necessary.” Meador recalls mattress assessments she has done where, upon testing the compression of the mattress, “fluids come out.” When incontinence is an issue, it’s important to be even more diligent with mattress and mattress cover checks.
Mattresses that are faulty are a portal for infection.

Anita Meador
Medline Senior Manager, Clinical Resources
The FDA reminds clinicians, “A hospital bed mattress cover provides outer protection to a mattress by preventing blood and other body fluids from entering the inside (inner core) of the mattress.”4 When mattress covers wear out, they no longer provide this protection, and body fluids can leak out, presenting risk of infection.
It’s important to inspect mattress covers on a regular basis. Using a mattress that has a cover that resists harsh chemical damage can help prolong the life of the cover and the mattress.
Key takeaway
Comprehensive inspection and timely replacement of medical mattresses is an important part of a prevention protocol. Clinicians should be able to recognize signs of mattress failure, and facilities should have a process to replace worn mattresses. Being proactive can help keep patients and residents safe.
References:
- Data on file
- Data on file
- Haesler, E. (2019). Prevention and Treatment of Pressure Ulcers/Injuries: The International Guideline 2019: Clinical Practice Guideline
- Center for Devices and Radiological Health & Center for Devices and Radiological Health. (2017b). Covers for Hospital Bed Mattresses: Learn How to Keep Them Safe. U.S. Food And Drug Administration. https://www.fda.gov/medical-devices/hospital-beds/covers-hospital-bed-mattresses-learn-how-keep-them-safe



