Vascular access team creation: How you contribute as an IP
Who’s inserting a central line and doing PICC line care at your facility?

Who needs a vascular access team? Your facility probably does. Most people admitted to hospitals require a vascular access device (VAD). In fact, hundreds of millions of VADs are inserted annually in the US.1
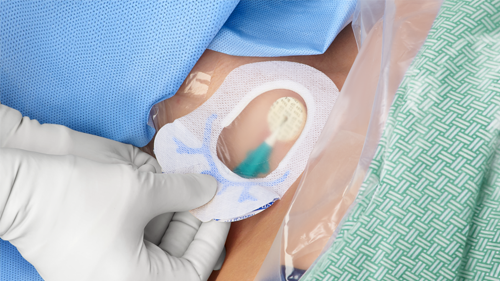
VADs include peripheral intravenous catheter (PIVC), midline, peripherally inserted central catheter (PICC), central venous catheter (CVC), tunneled CVC, subcutaneous port, arterial catheter and more.2 They all come with the risk of healthcare-associated infections (HAIs) developing. Fortunately, having dedicated personnel trained in providing advanced vascular access care facilitates a widespread improvement in patient outcomes, as well as reduced device-related complications.3
Where does an infection preventionist (IP) fit into the mix when it comes to building and maintaining a vascular access team? Let’s take a look at four areas where IP involvement is key.
1
Determine the need for a vascular access team
IPs can help assess various factors that affect patient safety, quality of care and resource utilization. Specifically:
- Review relevant data: Identify the incidence of healthcare-associated infections (HAIs) related to VADs in the facility. For example, look at data on the frequency of bloodstream infections and catheter-related infections, as well as other complications associated with VADs.
- Evaluate the current approach to VAD management: Review policies and procedures related to device selection, insertion, maintenance and removal, as well as the training and education provided to healthcare staff. In addition, assess the resources available for managing VADs, including staffing levels and equipment.
- Identify opportunities for improvement: Look at gaps in training and education, inconsistencies in policies and procedures, and issues related to resource utilization.
- Calculate the benefits of a vascular access team: Review your opportunities for improvement and determine if establishing a dedicated vascular access team would help you reach goals. Objectives include improved patient outcomes, reduced healthcare costs, and enhanced staff efficiency and satisfaction.
- Develop a plan for implementation: Put together an implementation plan that includes staffing levels, roles and responsibilities, policies and procedures, education and training, and performance monitoring and evaluation.
“Infection preventionists have knowledge and expertise that are instrumental in supporting the creation of a vascular access team,” says Donna Matocha, DNP, MSN, VA-BC, Medline Manager of Clinical Resources—Acute Care. “They can help management understand the need to spend money for this team. IPs have the data to support it.”
Studies show that training vascular access specialists increases first-time success and decreases costs.3
2
Create a vascular access team
Next, you’ll build the team, taking these four steps:
- Define staffing levels along with roles and responsibilities: Consider the number of patients requiring vascular access, the types of procedures being performed, and the current workload and demands on caregivers. Review relevant guidelines and recommendations from professional organizations such as the Infusion Nurses Society (INS) and the Centers for Disease Control and Prevention (CDC). These guidelines can provide recommendations on staffing levels and roles for vascular access teams based on best practices and industry standards.
- Develop policies and procedures: Work with other members of the healthcare team to develop policies and procedures related to vascular access device insertion, maintenance and removal. This can include guidelines for hand hygiene, skin preparation, device selection and dressing changes.
- Provide education and training: Educate healthcare staff on the proper insertion and maintenance of vascular access devices, as well as the prevention of infections associated with these devices. This can include providing updates on evidence-based practices, sharing best practices and providing feedback on compliance with infection prevention protocols.
- Monitor and evaluate: Track the incidence of HAIs related to vascular access devices and provide feedback to the vascular access team and other healthcare staff. This can help identify areas for improvement and promote a culture of safety. Monitor patient outcomes, staff satisfaction, compliance with protocols and other relevant metrics to assess the impact of the team and make adjustments as necessary.

A closer look at vascular access team members
The members of a vascular access team may vary depending on the specific needs and resources of the hospital but typically should consist of healthcare professionals with specialized training and expertise in vascular access device management. For example:
- Vascular access nurse: A registered nurse who has specialized training and expertise in vascular access device insertion, maintenance and removal. They may serve as a team leader or coordinator
- Infectious disease specialist: A physician who has specialized training in the diagnosis and treatment of infections, particularly those related to vascular access devices
- Clinical nurse specialist: A registered nurse who has specialized training in a particular area of nursing, such as critical care or infection prevention and control, and can provide expert guidance to the team
- Pharmacist: A licensed healthcare professional who can provide expertise in medication management related to vascular access devices
- Radiologist: A physician who specializes in the use of imaging techniques to guide the insertion and maintenance of vascular access devices
- Clinical engineer: A healthcare professional who can provide technical expertise in the selection, use and maintenance of medical devices, including vascular access devices
- Respiratory therapist: A licensed healthcare professional who can provide expertise in airway management and the use of mechanical ventilation in patients with vascular access devices
- Physical therapist or occupational therapist: A licensed healthcare professional who can provide expertise in the assessment and management of patient mobility and functional status related to vascular access devices
- Patient and family representative: A patient or family member who can provide feedback and input on the patient experience related to vascular access device management
Studies show that training vascular access specialists increases first-time success (FTS) and decreases costs and delays.3
3
Incorporate customized central venous catheter bundles into your protocols
Using customized central venous catheter (CVC) bundles can contribute to the success of the vascular access team. For example, insertion and maintenance bundles help:
- Standardize care: CVC bundles provide a standardized approach to the care of patients with CVCs, which can help to ensure consistency in the use of evidence-based practices across different healthcare providers and settings.
- Promote evidence-based practices: CVC bundles are based on evidence-based practices that have been shown to be effective in reducing the risk of CLABSIs. The use of evidence-based practices can improve the quality of care and patient outcomes.4
- Provide multimodal strategies: CVC bundles typically include multiple components, such as hand hygiene, skin preparation, use of aseptic barriers and daily assessment of the need for the catheter. These multimodal strategies work together to help reduce the risk of central line-associated bloodstream infections (CLABSIs).4
4
Partner with your medical supplier
Your medical supplier can help optimize the use of vascular access devices. Here’s how:
- Product selection: Your team can work with the supplier to select appropriate vascular access devices based on patient needs, provider preferences and product performance. They also can access information about new products, compare product features and make informed decisions about product selection.
- Product education: You can join forces with the medical supplier on providing education and training to the vascular access team on the proper use and care of vascular access devices. Options include in-services, webinars and other educational resources. By partnering with the medical supplier, the vascular access team can stay up-to-date on the latest product developments and best practices for device management.
- Product evaluation: Supply specialists can help you evaluate the performance of vascular access devices in real-world settings. This can involve collecting data on device performance, providing feedback to the medical supplier and participating in product trials.
- Supply chain management: Your supplier can help ensure that appropriate supplies and equipment are available when needed. Rely on them to monitor inventory levels, provide just-in-time delivery and manage the supply chain.
“IPs can provide just-in-time education,” says Matocha. “If a component needs to be added to the bundle, they can partner with the supplier and train staff on the change. Maybe there’s a device-related issue or a unit-based issue. They can work with the team and supplier to figure out next steps so they are continually driving toward or maintaining zero infections.”
Key takeaway
Vascular access devices, which are used on most hospital patients, open the door to the risk of an HAI developing. Using a vascular access team approach has been shown to improve patient outcomes. Infection preventionists play an important role in determining the need for a vascular access team, building the team, incorporating CVCs in the protocols and partnering with the hospital’s medical supplier—all to prevent HAIs.
References:
- Carr, P. (2018, March 20). Vascular access specialist teams for device insertion and prevention of failure. Cochrane Database of Systematic Reviews, 3(3). https://pubmed.ncbi.nlm.nih.gov/29558570/
- Moreau, N. (2020, May 12). Establishing Vascular Access Teams for Patient Safety. Infection Control Today, 24(4). https://www.infectioncontroltoday.com/view/establishing-vascular-access-teams-patient-safety
- Bell, J., Spencer, T. (2020, June 2). Implementing an emergency department vascular access team: A quality review of training, competency, and outcomes. The Journal of Vascular Access, 22(1). https://journals.sagepub.com/doi/10.1177/1129729820924554
- The Joint Commission. (2013, November 20). Preventing Central Line-Associated Bloodstream Infections: Useful Tools, an International Perspective. https://www.jointcommission.org/-/media/tjc/documents/resources/clabsi/clabsi_toolkit_tool_3-18_cvc_insertion_bundles.pdf