CAUTI in hospitals: Urinary catheter best practices vs reality
Learn why nursing protocols matter, bladder scanners are vital—and more.
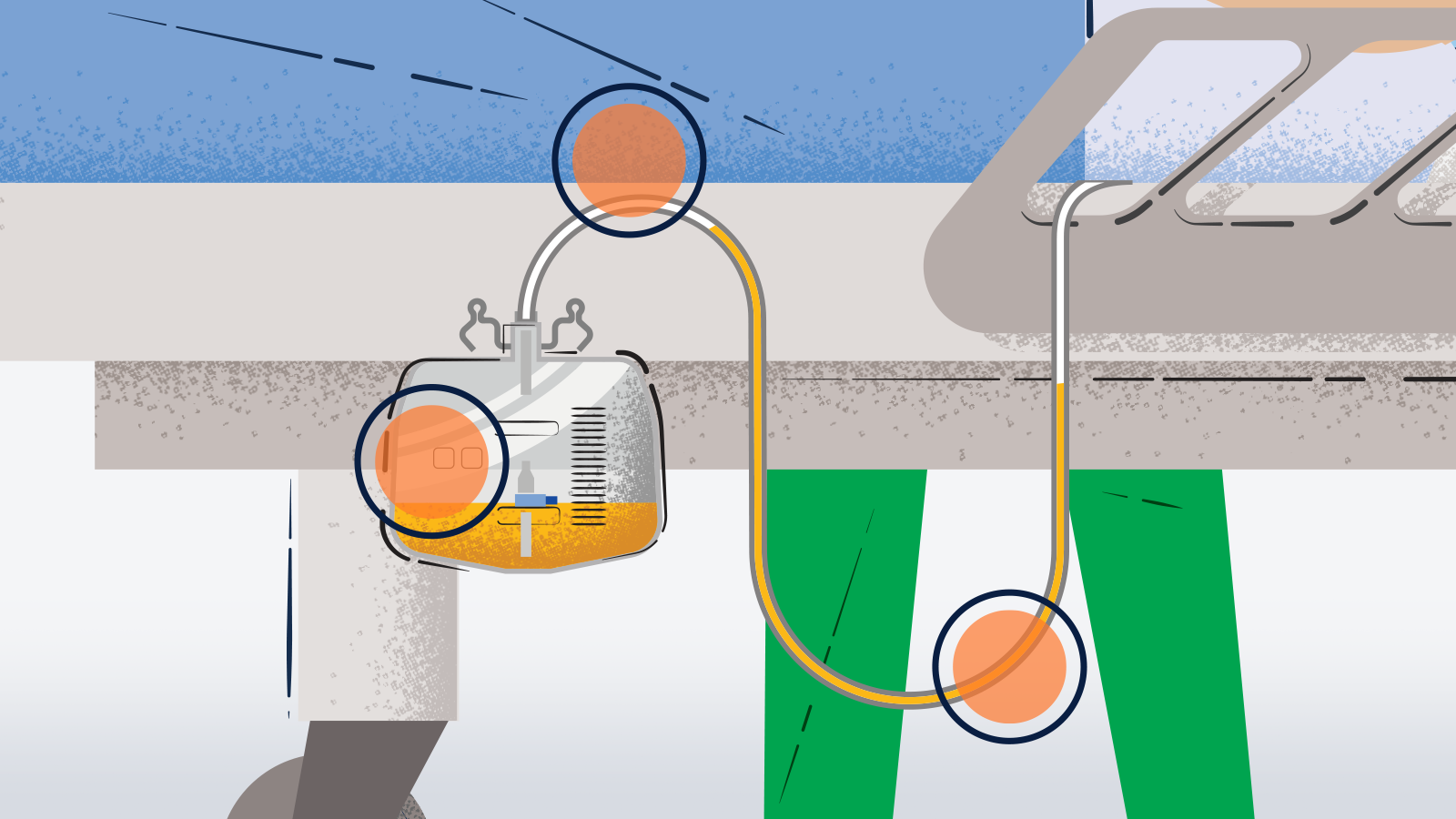
Catheter-associated urinary tract infection (CAUTI) has been associated with increased morbidity, mortality, hospital cost and length of stay. This is a big issue, considering that 15% to 25% of hospitalized patients may receive short-term indwelling urinary catheters (IUCs). In many cases, catheters are placed for inappropriate indications, and caregivers often are unaware that their patients have catheters, leading to prolonged, unnecessary use.1
In other words, it can be challenging for clinicians to follow best practices every time.
In 2022, Medline wanted to gain a better understanding of urinary catheter practices in US hospitals, so we:
- Completed practice audits of more than 2,500 IUC placements at multiple hospitals2
- Conducted staff surveys about these practices at multiple hospitals and received more than 2,100 responses2
What are the results of the audits and surveys? Download this infographic to learn current realities of urinary catheter practices—and where you may want to focus education and training to reduce CAUTI.
References:
- Centers for Disease Control and Prevention. Infection Control/Catheter-Associated Urinary Tract Infections/Background. Retrieved May 4, 2023, from https://www.cdc.gov/infectioncontrol/guidelines/cauti/background.html
- Data on file.





