Skin care to prevent pressure injuries: What the experts say
5 evidence-based tips for a more proactive regimen.
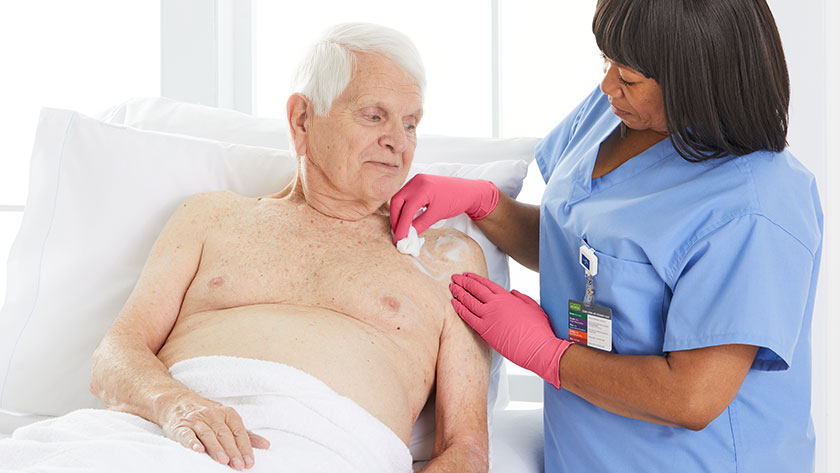
You know how important it is to be proactive about skin care to prevent pressure injuries (PIs).
7 to 10 days
is how long PIs can prolong a hospital stay.
3 times
more likely that PI patients will need long-term care once released.
It’s challenging when you’re short on staff and time. Plus, many caregivers may feel unsure about what skin care products to use depending on the skin condition.
That uncertainty motivated the Coalition for At-Risk Skin (CARS) to expand on the skin care guidance issued by the National Pressure Injury Advisory Panel (NPIAP).
They issued consensus statements after they saw concerning data that moisturizers and barriers weren’t being used as often as they should in some facilities.
According to the latest guidelines from both these leading expert panels, you can get a head start on skin health with the following evidence-based tips.
1
Apply moisturizer twice a day—and in the correct quantity
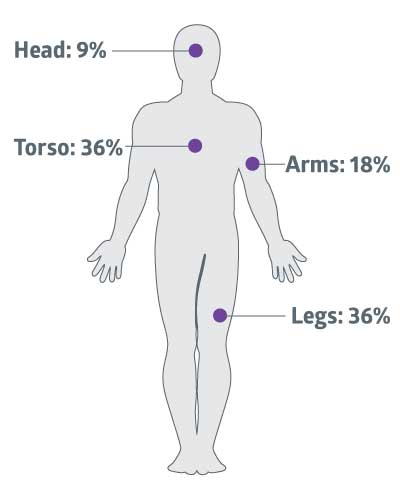
- CARS consensus statement #11: The approximate amount needed for a single application of moisturizer to the entire standard sized adult body is 30 grams or one ounce.
- CARS consensus statement #10: For individuals with at-risk skin, a moisturizer should be applied daily at a minimum and always after bathing. Twice daily moisturization has been demonstrated to show additional benefits.
With the data on inconsistent use of moisturizers, it’s helpful to keep best practices around this product top of mind. The diagram shows how much product to apply to each area of the body based on the CARS recommendation.
One reason caregivers may not be using moisturizers consistently is that staff are overworked, which makes it harder to provide product training. Newly hired or traveling nurses may need product training, and if a facility has a large skin care formulary, it can be even more time-consuming to coordinate.
Skin creams with pump dispensers can help your team use the correct amount. Each pump releases a consistent quantity so that it’s simpler to train everyone on how many pumps it takes to dispense an ounce.
2
Look for clinically effective ingredients designed to work for all skin types to improve outcomes
- CARS consensus statement #7: The properties, ingredients, utilization and intended use of skin care products impact their efficacy. This includes moisturizers and skin barriers.
- NPIAP guideline 3.1: Implement a skin care regimen that includes avoiding the use of alkaline soaps and cleansers.
Frontline staff want clinically effective ingredients that are shown to protect vulnerable skin. So which ingredients are effective, and which aren’t?
CARS advises you to use moisturizers and skin barriers with these ingredients:
- Dimethicone: Silicone polymer that’s an excellent skin protectant and is well tolerated by compromised skin and sensitive facial skin.
- Glycerin: Natural skin humectant that prevents moisture loss and supports proper skin function.
- Phospholipids: Class of lipids that support skin’s natural barrier function.
- Oleosomes: Micron-sized spheres of emollient plant oils to provide lasting moisturization.

They also recommend that you look for skin care products without parabens, fragrances, dye or aloe. You can follow NPIAP guidance by choosing pH-balanced cleansers over alkaline ones.
It’s helpful to find a comprehensive system of products that makes it as effortless as possible for caregivers to follow the CARS and NPIAP recommendations.
Case study: Leading long-term care facility decreases PIs by 62% with new skin care regimen
Mainstee County Medical Care Facility switched to a new system of products that made it easier for their team to follow skin care best practices. As a result, they improved outcomes.
- Switched to nutrient-rich line of cleansers, moisturizers and protectants by Medline Remedy®
- Reduction in hospital-acquired pressure injuries (HAPIs) by 62%
- Reduction in skin tears by 16.7%
While the clinical efficacy of ingredients is the most important factor to consider, there are other ways the formulas of moisturizers, barriers and cleansers can support healthy skin.
Studies have shown formulations that work for everyone—all skin types and tones, ages and acuity levels, as well as damaged or intact skin—save time and help caregivers use the correct product.
You can also look for formulas that are safe for everyone to use:
- CHG-compatible
- Hypoallergenic
- Alcohol-free
Additionally, patients tend to feel good about their care when products have a pleasant scent, texture and consistency.
3
Use creams and ointments over lotions
- CARS consensus statement #7: The properties, ingredients, utilization and intended use of skin care products impact their efficacy. This includes moisturizers and skin barriers.
- NPIAP guideline 3.1: Implement a skin care regimen that includes avoiding the use of alkaline soaps and cleansers.
For optimal skin health, hydration is key. An important insight that CARS found through their research is that lotions don’t work as well as creams or ointments. Why? Lotions may contain more dehydrating ingredients, putting skin at risk for transepidermal water loss (TEWL). TEWL weakens skin’s barrier function.
Another way that creams benefit at-risk skin is that they spread easily and are aesthetically pleasing. Ointments are helpful whenever caregivers need to hold moisture in the skin for prolonged periods of time or want to protect open skin.
4
Select a unified skin care system that empowers caregivers to deliver their best care
You want to make it as simple as possible for frontline staff to follow skin care best practices, but where do you start?
Vendors can help. They have a role to play in helping caregivers feel more confident about using skin care and following expert recommendations.
Patricia Turner, BSN, RN, CWOCN, CWS and Medline Director of Clinical Resources Skin Health, agrees that vendors should create skin care products that help caregivers keep up with an evidence-based regimen. “It’s all about safety nets to make sure that clinicians can’t make a mistake,” says Turner.
“It’s all about safety nets to make sure that clinicians can’t make a mistake.”

Patricia Turner
BSN, RN, CWOCN, CWS, Medline Director of Clinical Resources Skin Health
Vendors can create skin care systems that put that safety net in place. It starts with observing and listening to caregivers during the product design phase.
Case study: Ohio health system reduces costs with a unified skin care system
OhioHealth wanted to reduce variations across 9 nursing units in 6 hospitals. They reduced costs and improved caregiver satisfaction with the Medline Remedy system.
- Reduced skin care formulary from 13 products from different companies to 7 Remedy products
- Cost savings of $40,000 annually with this unified product line.
- Staff can more easily identify the correct product for a clinical use with color-coded packaging and educational materials of the Remedy system.
- Staff prefer clear, accessible educational materials to other vendors
When Josh Kolof, Director of Product Management at Medline, and his team were updating their skin care system, they worked closely with caregivers to understand their challenges.
They found that they could support frontline staff with a comprehensive skin care system that helps by:
- Cutting down on the formulary size, simplifying the coordination of in-service training
- Using color-coded packaging so that caregivers can easily associate colors with clinical uses and quickly pick out the product on a shelf
- Using clear, directional product names that indicate their clinical use
- Putting how-to videos and color-coded educational materials that correspond with packaging colors at their fingertips
Medline Remedy® redefined: Spotlight on the relaunch
Recently, through close work with advisory boards and clinical groups, the Remedy line was redesigned. The trusted formulas remain the same, but the product packaging and names were updated to be even more caregiver-friendly.

A comprehensive system of products can help you standardize care and follow evidence-based guidelines, which can improve skin health and reduce costs. That’s helpful when so many facilities are being asked to do more with less.
5
Cleanse the skin properly and use preventative barrier after every incontinent episode
- NPIAP guideline 3.1: Implement a skin care regimen that includes cleansing the skin promptly after episodes of incontinence.
- CARS consensus statement #12: Skin barrier products are recommended when moisture, microclimate, friction and shear are contributing factors to at-risk skin.
Excess moisture is one of the forces that leads to pressure injuries. Experts agree that it’s important to manage moisture as part of a skin care regimen to prevent breakdown.
That’s why it’s important to cleanse the skin and apply a barrier product after every incontinent episode.
Key takeaway
Data shows that caregivers may not be using skin care consistently. As a result, facilities are looking for more guidance on products and how to use them. The evidence-based tips in this article address the best ways to use skin care to prevent pressure injuries. Fortunately, several facilities successfully used a comprehensive skin care regimen to improve outcomes, save nursing time and reduce costs. Look for a system like Medline Remedy that makes it easier for caregivers to follow best practices.