How effective is the environmental cleaning in your LTCF?
Learn how to go beyond nursing home housekeeping to help improve safety.

You’re working every day to build a strong team defense in the fight against healthcare-associated infections (HAIs). How do you determine weaknesses? To help identify gaps in infection control practices, Medline completed “discovery assessments” with more than 100 long-term care providers across the nation in late 2022.
The goal being, once you assess your risk level, you’re better informed and armed to close those gaps through education, training and other viable solutions.
This article is the third in a five-part series on how to address each of the main infection control challenges identified.
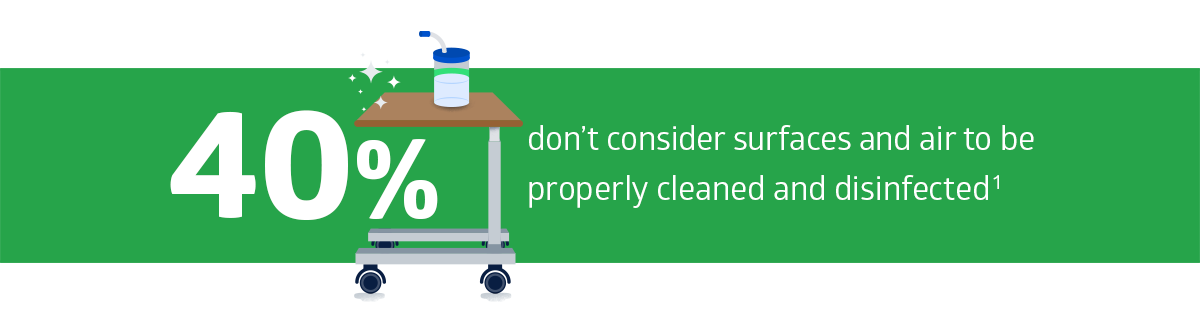
So what did the assessment results show? We asked LTC leaders, “Thinking about your organization, how well do you consider surfaces and air to be cleaned and disinfected?” Here’s what we learned:
This is a big issue: Many pathogens responsible for outbreaks and HAIs can be spread by contaminated surfaces.2 In addition, multidrug-resistant organisms (MDROs) are on the rise, with Candida auris spreading at an alarming rate in US healthcare facilities in 2020-2021.3
Following are five approaches to raising environmental services (EVS) levels in your facility:
Partner with your EVS director on environment of care protocols
As an infection preventionist, you oversee your facility’s entire infection prevention and control (IPC) program. That includes providing a clean and sanitary environment for residents, staff and visitors.
Where do you start?
Break down silos and get to know your EVS director. Meet regularly and build trust. Your EVS director should feel comfortable going to you for help and saying, “I’m thinking about making this decision. I’d love your input.”
Together you can develop appropriate protocols, processes and guidelines for cleaning and disinfection of surfaces and air. Keep in mind:
- Processes and products should be evidence-based, designed specifically for healthcare and safe for EVS frontline workers to use
- Your protocols should include ongoing staff training and education
- You need to include methods for monitoring and measuring cleanliness and staff performance, as well as providing immediate, non-punitive feedback
- Resident and family involvement are key to a safe environment
Let’s take a closer look at these components and how you can collaborate with EVS leadership and staff.
Match your protocols and products to your facility’s needs
First, recognize the difference between “housekeeping” and “environmental services.” While housekeeping staff focus on tidying and cleaning, EVS staff are highly trained to clean and disinfect medical equipment, patient and resident rooms, and common areas within healthcare facilities.
“EVS focuses a lot more on the science behind disinfectants and knowing the chemical composition of the products they’re using, to make sure that they’re properly cleaning and disinfecting a facility,” says Caryn Arnold, MBA, RN, BSN, CNOR(E), a-IPC, Medline Medical Science Liaison.
To help EVS staff, your protocols should include a clean-by-sequence process that effectively addresses the high-touch surfaces recognized by the Centers for Disease Control and Prevention (CDC) that are most vulnerable to the spread of pathogens.
Why is sequence important?
More than 90% of high-touch surfaces in long-term care facilities, including handrails and equipment controls, are contaminated with fecal matter and other potential sources of infectious disease spread, according to a study released in 2022.4
“When you’re making a product selection, there are a lot of factors and criteria to consider,” says Megan Henken, Medline Vice President of Product Management. “You need to look at efficacy—what pathogens a product kills. And you need to know the contact times for each product.”
Finally, boost EVS efforts by including a portable air disinfection system in your protocols. Some of today’s ultraviolet (UV) light decontamination devices are more affordable and safe to use in occupied resident rooms.
More than 90% of high-touch surfaces in long-term care facilities are contaminated with fecal matter and other potential sources of infectious disease spread3
Provide staff education and training that engage and resonate
All EVS staff should understand proper cleaning and disinfection techniques. This includes the use of personal protective equipment (PPE), proper dilution of cleaning and disinfection products, and hand hygiene.
“Staff also need to understand the ‘why’ behind the ‘what’ and ‘how,’” says Henken. “They need to know what pathogens are, how long they can survive on a surface, how they reproduce, how they can be transmitted from one surface to another and how those pathogens transfer to people and potentially cause infections.”
In other words, explain how their work contributes to the overall health and safety of everyone in the facility. And how much they are valued and appreciated.
At the same time, it can be challenging for EVS staff to learn everything. They don’t have a healthcare background and many team members speak English as a second language. Here are some strategies that may help:
- Use simple language when discussing the importance of cleaning and disinfection. Avoid technical terms or jargon that may be difficult for non-native speakers to understand.
- Use visual aids, such as pictures, videos, and infographics, to help explain the concepts visually. These can be especially helpful for staff members who have difficulty understanding written or spoken English.
- Provide multilingual resources, such as training materials, posters and signs, to help staff members who may have difficulty understanding English. These resources should be available in the languages spoken by staff members.
- Provide hands-on training and demonstrations to help staff members understand the proper techniques for cleaning and disinfection. This can be particularly useful for staff members who have difficulty understanding instructions given in English.
- Encourage questions by staff members and provide opportunities for them to ask questions during training sessions. This can help to clarify any misunderstandings and ensure that staff members have a thorough understanding of the concepts being discussed.
Think of all they have to learn. Learning a few phrases in your staff’s native language would go a long way in building rapport and engagement.
Staff also need to understand the “why” behind the “what” and “how.”

Megan Henken
Medline Vice President of Product Management
Monitor, measure and provide feedback
As the infection preventionist, you should monitor adherence to the cleaning and disinfection plan. Methods can include directly observing cleaning practices and reviewing documentation of cleaning and disinfection activities.
To measure cleanliness, you can use surface cleaning-validation tools such as ATP testing. Results can be used to help spot problem areas.
When providing feedback to EVS staff during direct observation, make sure to praise them when they correctly follow processes. When improvement is needed, treat it as a non-punitive educational opportunity. Staff will be happy to learn and will feel more comfortable approaching you with any questions.
You’ll also provide feedback to the EVS director. You should be meeting regularly, whether one on one or as part of a committee. Make sure to review and revise protocols as needed. This can include updating the list of high-touch surfaces, adjusting the frequency of cleaning and disinfection based on infection rates, and incorporating new products or techniques.
Educate residents and their families on the importance of EVS
A recent study shows that EVS cleaning rates are lower for semi-private rooms and rooms where residents are present.5 Involving residents and family caregivers in the EVS process can help ensure that everyone is on the same page and working together to maintain a clean and safe environment.
“EVS staff may be uncomfortable entering rooms when residents and/or family members are present,” says Arnold. “Staff should be encouraged to introduce themselves and explain what they’ll be doing.”
You can help residents and family caregivers understand the importance of EVS by providing tent cards, brochures, posters and informational sessions.
When residents and their families are educated, they’ll be more likely to:
- Communicate concerns regarding the cleanliness of resident rooms. This can include reporting any spills, stains or other issues that may need attention.
- Keep rooms clutter-free so EVS staff can clean and disinfect the room thoroughly.
- Follow instructions given by EVS staff regarding cleaning and disinfection practices. This can include properly disposing of trash and ensuring that surfaces are clear for cleaning.
- Assist with cleaning by wiping down surfaces with disinfectant wipes.
In addition, they can provide feedback to EVS staff, letting staff know if they notice any areas that may have been missed during cleaning.
Key takeaway
With MDROs on the rise, EVS plays a bigger role than ever in providing a clean, safe environment. When you partner with your EVS director; have the right protocols, processes and products in place; provide training and education; monitor, measure and provide feedback; and involve residents and family caregivers, you’ll be well positioned to raise EVS levels in your facility. Stay tuned for the fourth installment of this article series.
References:
- Medline 2022 Long-Term Care Discovery Assessment Findings. Data on file.
- Martonicz, T. (2023, March 16). IPs’ Challenges With Facility Cleaning and Disinfection Programs. Infection Control Today. IPs’ Challenges With Facility Cleaning and Disinfection Programs (infectioncontroltoday.com)
- Centers for Disease Control and Prevention. (2023, March 20). Increasing Threat of Spread of Antimicrobial-resistant Fungus in Healthcare Facilities. https://www.cdc.gov/media/releases/2023/p0320-cauris.html#:~:text=Candida%20auris%20(C.%20auris),the%20Annals%20of%20Internal%20Medicine.
- Novotney, A. (2022, February 18). Nearly all high-touch surfaces in LTC are contaminated, study finds. McKnight’s Long-Term Care News. Nearly all high-touch surfaces in LTC are contaminated, study finds – Clinical Daily News – McKnight’s Long-Term Care News (mcknights.com)
- McKinley, L., et al. (2022, May 6). Evaluation of daily cleaning and disinfection practices in veterans affairs acute and long-term care facilities: A mixed-methods study. American Journal of Infection Control, 51(2), 205-213. https://www.ajicjournal.org/article/S0196-6553(22)00438-2/fulltext





