Is natural disaster preparedness in your response plan?
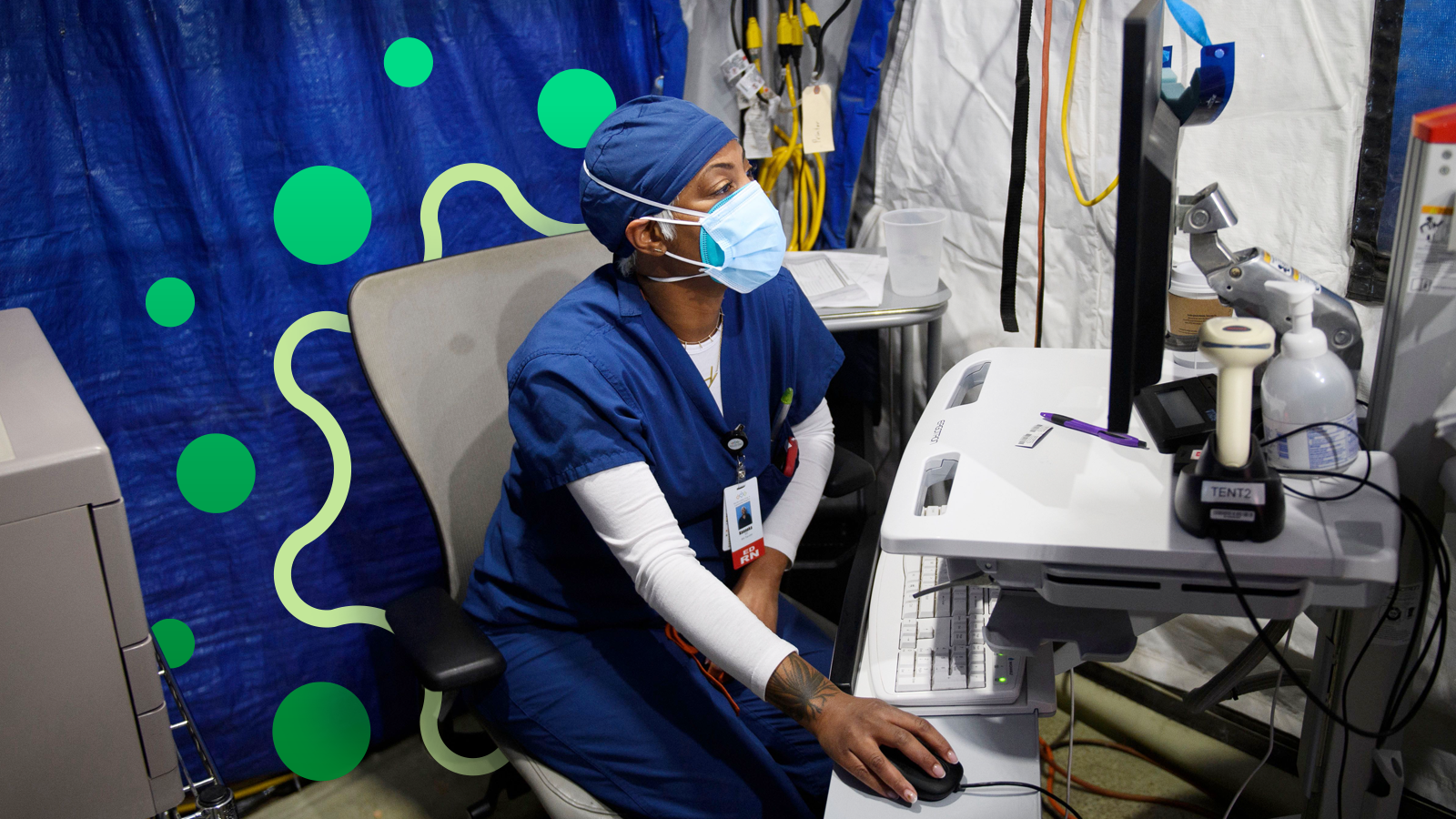
Infection preventionists are key to controlling post-disaster diseases.
Hurricane Katrina. The words make you think of people on top of their roofs, waiting to be rescued as water levels rose. They needed food, water and shelter.
But that’s not all. They needed treatment for whatever germs they picked up as they scrambled to escape the flood. What’s so different about these germs?
Must be something in the water
“We have to have clean water,” says Donna Matocha, DNP, MSN, VA-BC, Medline Manager of Clinical Resources—Acute Care. “During natural disasters, infrastructure often is damaged and sewage and clean water systems can fail. So we have contamination.”
Floodwaters can contain downed power lines, human and livestock waste, hazardous waste, debris, rodents, snakes and more.1
Add to that people being displaced from their homes, overcrowding in shelters and makeshift care sites, poor sanitation conditions and injuries.2
“We can’t bathe ourselves or clean our hands properly,” says Matocha. “We can’t wash our food properly. And stagnant water takes a while to drain, making it a breeding ground for mosquitoes that harbor disease.”
What can result? Infectious diseases including diarrheal diseases, acute respiratory infections, malaria, leptospirosis, measles, dengue fever, viral hepatitis, typhoid fever, meningitis, as well as tetanus and cutaneous mucormycosis.2
Floods are the most common natural disasters worldwide, coming in at 40%. They can take out infrastructure and lead to communicable diseases—days, weeks and sometimes months after the start of the disaster.2
How do you stop the spread?
Hospitals and infection preventionists (IPs) need to have a strategy to prevent disease transmission in the facility and the community as they respond to mass casualty events.
We have to have clean water. During natural disasters, infrastructure often is damaged and sewage and clean water systems can fail. So we have contamination.

Donna Matocha, DNP, MSN, VA-BC
Medline Manager of Clinical Resources—Acute Care
This infection prevention strategy should be included in the hospital’s overall emergency management plan and align with the four phases of emergency management:3
- Mitigation: Actions to either prevent or reduce illness/injury and death as well as ease the economic and social impact of the event on the affected community.3 This may include conducting risk assessments to identify potential natural disasters the community may face, the infectious diseases that could result and how to treat them, and the number of casualties that may occur.
- Preparedness: A plan that involves all of the measures taken to prepare for an emergency and educate the workforce.3 Actions include ensuring access to appropriate personal protective equipment; having supplies of medications that may be needed; identifying where patients can be isolated; and collaborating with other healthcare facilities, public health departments, first-responders and community officials to determine who takes in patients from the disaster first, who gets overflow, where triage can be performed and where shelters can be set up.
- Response: Occurs after the disaster strikes when the plan developed in the preparedness phase is implemented.3 Response efficiency hinges on having a strong command center and appointed spokesperson, providing ongoing internal and external communication to advise of disease updates and collaborating with first-responders so they know where to bring people who may have an infectious disease.
- Recovery: Actions needed to return a facility and/or community to its pre-disaster point as soon as possible. By educating the public and staff about symptoms of potential infectious diseases, hospitals and IPs can contribute to lowering the risk of disease outbreaks months after the disaster.3
The IP plays a major role in the strategy
IPs need to be involved in assessing all aspects of readiness for mass casualty events in regard to potential disease transmission. Their input is needed for:
- Having around the clock infection control coverage
- Strategies for receiving and posting health alert messages within the facility
- Patient management
- Food safety
- Water management
- Sanitation control
- Environmental decontamination
- Development of crisis standards of care that affect infection transmission
- Prioritization for limited supplies of anti-infective therapy
- Screening/triage protocols
- Occupational health/safety procedures
- Outbreak investigation coordination3
In addition, community disaster planners will need guidance by IPs when setting up and running care sites and shelters for displaced people.3
40% of natural disasters worldwide are floods2
IPs need to have an internal communication plan to inform all healthcare facility staff, patients and visitors about infection prevention strategies that need to be implemented. Examples include screening measures/procedures; the need for and appropriate use of isolation precautions, PPE, hand hygiene and social distancing practices; and post-exposure follow-up.3
In addition, IPs need to be involved in the development of crisis standards of care. Resources start to dwindle during mass casualty events. Tough decisions need to be made regarding how to allocate limited numbers of ventilators or medications, where contagious patients will be housed if all isolation rooms are full, which staff will be given PPE if stocks become depleted and how to safely reuse respiratory protection when necessary.3
Finally, a natural disaster resulting in sheltered people displaced by the event requires vigilant surveillance on all fronts. IPs should communicate information gathered from the screening process and outbreak investigation to local public health officials.3
Key takeaway
Natural disasters can lead to a host of infectious diseases, even months after the start of a disaster. It’s important that a hospital’s emergency response plan include a strategy for infection prevention to treat patients and control the spread of these diseases. IPs play a significant role in developing and implementing the strategy, including serving as a consultant to internal and external partners.
References:
- CDC. Natural Disasters and Severe Weather/Floodwater After a Disaster or Emergency. Floodwater After a Disaster or Emergency | CDC
- Kuadio, I., et al. (2014, January 10). Infectious diseases following natural disasters: prevention and control measures. Expert Review of Anti-Infective Therapy, 10(1), p95-104. Full article: Infectious diseases following natural disasters: prevention and control measures (tandfonline.com)
- Rebmann, T., and The 2008 APIC Emergency Preparedness Committee. (2009, March 24). APIC State-of-the-art Report: The role of the infection preventionist in emergency management. American Journal of Infection Control, 37(4), p271-281. APIC State-of-the-art Report: The role of the infection preventionist in emergency management – American Journal of Infection Control (ajicjournal.org)





