Making it personal: How standardization and personalized care work together
Critical thinking is key to treating the individual within your protocols.

Most healthcare organizations—and clinicians—agree: standardized care is best practice. Care consistency helps improve outcomes. And it’s a more efficient and cost-effective way to work. But every patient and every resident are different. So how do you standardize care and make it personal?
Some may think standardized and individualized care are at odds, but the truth is, they’re closely connected.
All facilities benefit from standard clinical protocols, but that doesn’t mean that caring for patients and residents takes a one-size-fits-all approach. Within these established protocols, caregivers should consider the individual’s needs, preferences, history and ability to adhere to the treatment plan.
“Without standardization, there’s chaos,” says Medline Clinician Katie James, BA, RN, CWCN. But she adds, “Frontline staff still have the critical thinking skills to individualize care within the established standard of care.”
“Frontline staff still have the critical thinking skills to individualize care within the established standard of care.”

Katie James
BA, RA, CWCN and Medline Clinician
Even within skin and wound care—a highly standardized area with evidence-based best practices—there’s room to customize. Many wound care nurses have a saying, “Don’t just treat the hole in the patient, treat the whole patient.”
Let’s look at how to empower clinicians to standardize care while being mindful that every person is different.
One good turn deserves another: Individualizing an NPIAP protocol
Ever since Florence Nightingale was making her rounds in the 19th century, caregivers have been advised to turn patients every two hours. That is until 2019—the year when the NPIAP updated their guidelines to say that the turning frequency should be determined on an individual basis. The NPIAP now recommends caregivers factor in the person’s activity levels and ability to reposition themselves. Based on individual needs, caregivers may find that some people need be turned more frequently than every two hours.
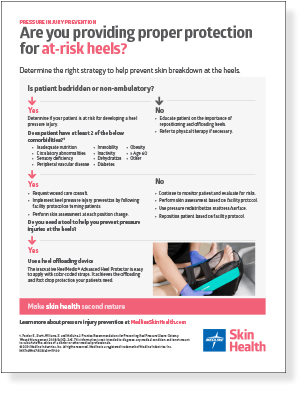
As facilities work to support staff to make the right decision about this and other protocols, education and training can help enhance caregivers’ critical thinking skills and build confidence. Informative and easy-to-use resources like decision trees are also beneficial. For example, this decision tree empowers clinicians to choose and properly use the right heel protection to help prevent pressure injuries.
Improving patient adherence and outcomes
The treatment plan recommended by the clinical protocol is always the best plan. But what do you do when a patient or resident can’t or won’t follow the recommended treatment?
When it comes to managing venous disease, the recommended level of compression is 30-40 mm Hg, but some patients can’t tolerate it.
In those cases, clinicians typically step down the compression until they find a level that’s more appropriate for the individual, ensuring better adherence and outcomes.

Sometimes, it’s not clear why a patient or resident isn’t following their recommended treatment. In these cases, CNAs can provide helpful insights about the individual needs, preferences, and habits of the people they care for every day.
Individualizing skin care within a standardized product formulary
Variations in products lead to variations in care. That’s why a simplified product formulary makes it easier for caregivers to provide their best care. One way facilities can drive standardization is by limiting themselves to one product per clinical use. So, it’s key to make product choices that ensure every patient and resident gets the proper treatment.
A facility may have a standard for bathing bed-bound patients, but what makes an individual feel clean and comfortable can vary from person to person. Some may feel clean after a sponge bath. Others may prefer to use cleansing wipes. Both accomplish the goal of keeping patient skin properly cleaned.

Regularly moisturizing skin is a best practice, and most facilities often have a standard, go-to moisturizer to help keep skin healthy. It’s important to consider the needs of the individual patient or resident, as well as the greater population the facility serves. So how do you simplify your product formulary and meet the specialized skin care needs of your facility’s population?
To provide the best care, partner with a supply vendor who can help you choose the right products to meet the needs of your patient population. Making a more intensive moisturizer the standard is especially important for facilities that serve populations with aging or darkly pigmented skin, which typically requires more moisturization.
Key takeaway
Every patient and every resident are different. Empowering caregivers to strike the right balance of standardization and personalized care can help drive better outcomes and patient adherence. A reliable clinical partner who offers best practice guidance supported by education and training, and a system of products can help bring it all together.
References:
- National Pressure Injury Advisory Panel, Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline 2019, pages 89, 117