Wound measurement tools: Your guide to what works best
Compare 4 types of devices to help choose the right one for your wound care needs.

When it comes to measuring wounds, did you know the average accuracy rate among caregivers is only 34%?¹ Wound measurement is an important part of assessing and classifying wounds, but we understand that variation among caregivers is common. With the right tools, accuracy can improve significantly, studies show by nearly 70%.¹
In this article, we discuss the importance of accuracy in wound measurement and classification, the challenges, and pros and cons of various types of wound measurement tools. More accurate wound measurement helps lead to better wound management.
34%
Average accuracy rate in wound measurement¹
70%
Increase in accuracy with better tools and education¹
Why is wound measurement essential to wound care?
Measuring wounds is an important part of a structured and consistent approach to wound assessment for many reasons. Perhaps most importantly, it provides a tangible marker of wound healing. “It gives us a specific value and allows us to monitor and compare the wound at each assessment,” says Patricia Turner, BSN, RN, CWOCN, CWS, Medline Director of Clinical Resources Skin Health. “And this equates to knowing if your treatment is working,” she adds.
Another benefit of accurate and consistent wound measurement is “the potential or predictability of whether the wound will heal at all,” Turner explains, or whether it is considered a chronic wound. That’s why knowing the size of a wound and monitoring its changes is important to the healing process—it informs treatment decisions that help keep the wound on a path to healing.
Measuring wounds “gives us a specific value and allows us to monitor and compare the wound at each assessment.”

Patricia Turner
BSN, RN, CWOCN, CWS, Medline Director of Clinical Resources Skin Health
Without valuable wound data, there’s increased risk of delayed wound healing, pain, complications and decreased quality of life. Caregivers who have a reliable tool have a better chance at following best practices.
What are the challenges to consistent wound measurement?
Caregivers measure wounds on a daily basis, but, as Turner notes, “Wound measuring is still a very subjective task.” If every wound conveniently always took on the shape of a square, rectangle or perfect circle, measuring them would be much easier, right? But you know that’s not the case.
You might come across these additional challenges to accurate measurement:
- Different caregivers using different tools to measure the wound
- Determining and defining wound edges
- Confusing length for width in your calculation when measuring a wound that’s longer side to side
- Relying on size alone to define a wound instead of factoring in wound qualities, such as granulation tissue, tissue edema and necrotic tissue
- Measuring wounds that curve around areas of the body or occur in skinfolds or crevices
- Compromising accurate measurement due to stretching, separating or squeezing skin during assessment instead of keeping the body in a neutral position
Review your measuring techniques
There are different ways to approach wound measurement, including:
Head-to-toe: From this perspective, the length is always on a head-to-toe axis. Regardless of where the wound is located, the top of the wound is in line with the head of the patient, while the width would be in line with the patient’s arms if they were outstretched at the sides.
Clock methodology: Similar to the head-to-toe concept, caregivers envision a clock, with the length axis of 12:00 being at the person’s head, 6:00 at their feet and so on.
Length, width and depth: In this method, caregivers would measure the greatest length and the greatest width of the wound, at a 90-degree perpendicular angle from the length, to get an approximation of the surface area.
In the case of a deeper wound, a cotton swab would be used to measure depth and then calculate volume. Gently insert the cotton swab 90 degrees down to get to the deepest part of the wound.
Wound measurement tools: pros and cons
From the simple to the sophisticated, there are many tools for measuring a wound. Here, we round up some of the available tools so you can select the right tool for your needs and improve wound outcomes.
1
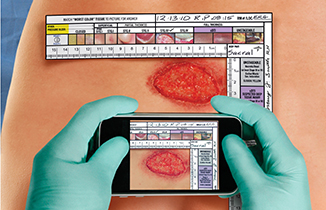
For high accuracy: digital imaging
The latest digital options use a smartphone application to gather images and data. Caregivers photograph, assess, document and share data in real time to customize treatment. The patented NE1 Wound Management System is a build on the paper version, enabling caregivers to securely upload images to electronic patient records for evaluation, documentation and tracking
Pros: More accurate wound measurement and classification helps stage wounds for proper treatment and reimbursement; product recommendations; less direct contact with the wound surface; inexpensive; remote assessment empowers caregivers not familiar with wound measurement, such as home health nurses
Cons: Curves in wounds may be difficult to photograph; some wounds may not fit in a single image; tunneling and undermining is entered manually

Future technology for measuring wounds includes 3D images, augmented reality and laser-generated models. Plus, medical devices such as the NE1 Wound Management System is expected to evolve to a point where artificial intelligence will assess the wound automatically. For now, research shows that digital imaging tools provide more accurate measurement and classification.
2
For irregular shapes: tracing sheet
These are typically either acetate sheets or transparent film. Caregivers place it on top of the wound and trace the wound edge with an indelible pen to measure the circumference. The tracing can then be placed on a paper grid with squares to calculate wound area. Often, two layers are used, so one can be tossed and the other placed on the grid.
Pros: Inexpensive; useful for irregular-shaped wounds
Cons: Accurate tracing is challenging; wound exudate may make it hard to see wound edges; tracing sheet can damage or deform the wound; tracing sheet gets contaminated in contact with wound; can be time-consuming; may be uncomfortable for the patient
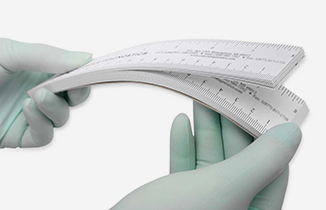
3
For descriptive info: ruler with context
In addition to measurement, these types of paper rulers may also include qualitative hints, such as color and thickness, which help classify the wound. One example, the NE1 Wound Assessment Tool has a vertical and horizontal ruler to allow for simultaneous measurement of both axis.
Pros: Inexpensive; easy to use at the bedside; gathers wound quality information to aid in assessment
Cons: Variation in measurement among caregivers is high
4
For tight budgets: paper ruler
These point-of-care disposable rulers typically come in large packs, like a pad. Formatted in centimeters, they usually include spaces to write in a patient’s name and the recorded measurements to use as reference in photos alongside the wound.
Pros: Inexpensive; small and light to carry; easy to use at the bedside; one-time use makes them more sanitary
Cons: Variation in measurement among caregivers is high
Key takeaway
Accurate wound measurement and assessment helps caregivers select the best treatment options, track healing and predict healing ability. While there are a wide range of measurement tools available, more advanced digital technology has advantages over more traditional methods, offering a more robust picture of each wound.
References:
- Young DL, Estocado N, Landers MR, Black J. A Pilot Study Providing Evidence for the Validity of a New Tool to Improve Assignment of National Pressure Ulcer Advisory Panel Stage to Pressure Ulcers. Advances in Skin & Wound Care. April 2011:(24)4:168-75.




