How ICU universal decolonization helps with MRSA prevention
Learn effective protocol elements such as CHG baths and nasal antiseptics.

On any given day in any given intensive care unit (ICU) across the country, nurses and other clinicians are caring for patients whose treatment may involve the use of medical devices like central lines, urinary catheters or ventilators. These lines and devices, plus a patient’s own surgical wounds and other breaks in the skin, pose enormous risk for infection.1
It’s why the ICU is top of mind among nursing leaders and infection prevention experts, who are continuously exploring new ways to prevent or reduce healthcare-associated infections (HAIs) in hospitals and health systems. Here is what we know:
- Methicillin-resistant Staphylococcus aureus (MRSA) is possibly the single most concerning HAI pathogen when it comes to harmfulness, pervasiveness, diversity of disease and the likelihood for widespread transmission.1
- Staphylococcus aureus is the most common cause of ventilator-associated pneumonia (VAP) and surgical-site infections (SSIs) and the second most common cause of central line-associated bloodstream infections (CLABSIs). Two-thirds of S. aureus HAIs were the result of MRSA.1
- The majority of HAIs are caused by bacteria, such as MRSA, that live on the skin and in the nose and enter the bloodstream, lungs and bladder by way of devices and incisions that have compromised the body’s natural barriers. These bacteria may be the patient’s normal flora, or they may be new, often antimicrobial-resistant organisms acquired during a hospital stay.1
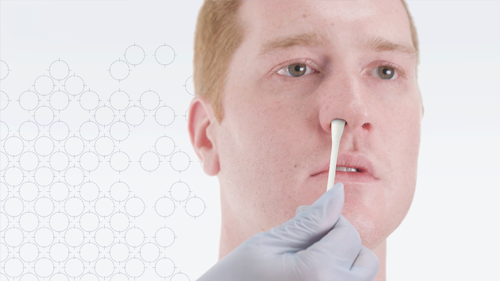
- The nose is a major reservoir of S. aureus, and use of antiseptic agents such as mupirocin, povidone iodine and ethyl alcohol are essential to killing these bacteria.1
- 20 billion microbes in our mouths reproduce every four to six hours. These pathogens can colonize and then be aspirated into the lungs, causing hospital-acquired pneumonia (HAP).2
- According to a worldwide ICU study, 18% of patients in 83 North American ICUs are infected by MRSA. Worse, studies have shown risk for infection can be as high as 33% among MRSA carriers a year after a patient has been hospitalized.1
Universal ICU decolonization and why it matters
Universal decolonization—the routine use of special soaps and nasal and oral antiseptics to reduce bacteria on the skin and in the nose and mouth—is proving to be the most effective way to reduce MRSA.1
So, what does a protocol for universal ICU decolonization look like? First, it should always include CHG bathing and a nasal decolonizer. Secondly, it should complement other infection prevention strategies, such as hand hygiene and environmental hygiene. Specifically, here is what a universal ICU decolonization protocol should look like:
- Use chlorhexidine (CHG) baths daily in place of bathing with soap and water for the duration of the ICU stay; also use only CHG-compatible lotions.
- Use a nasal antiseptic twice a day for five days during the ICU stay. Mupirocin is preferable, but if a patient is antibiotic-resistant, povidone iodine is the next best alternative. Also, ethyl alcohol is beginning to emerge in some studies as an acceptable alternative.
- Use a daily oral antiseptic for the duration of the ICU stay. This is especially important for patients who are at high risk for HAP2 and to prevent VAP.3
- Do not screen for bacteria unless required by law. Screening is not necessary with universal decolonization. Ending this process can reduce costs with the elimination of testing and, with that, the need for gloves and gowns.
What’s important to emphasize in a universal ICU decolonization protocol is that it must include both CHG bathing and a nasal decolonizer—the two work in tandem.

Joan Hebden, MS, RN, FAPIC, FSHEA
Clinical Consultant, Medline
What the research tells us
Protocols for universal ICU decolonization grew out of REDUCE MRSA (Randomized Evaluation of Decolonization vs Universal Clearance to Eliminate MRSA), a trial conducted in 2013 by the Centers for Disease Control and Prevention in partnership with the Hospital Corporation of American (HCA) and nearly four dozen of its affiliates. The 18-month trial compared three protocols:
- Individuals admitted to the ICU were screened and, if they had MRSA, were isolated.
- Individuals admitted to the ICU were screened and, if they had MRSA, were isolated and decolonized using CHG baths and mupirocin nasal antiseptic.
- No individuals admitted to the ICU were screened, and all were decolonized using CHG baths and mupirocin nasal anticeptic.
The trial found that daily CHG bathing and nasal decolonization twice a day for up to five days in all ICU patients reduced MRSA in clinical cultures by 37% and 44% in all-cause bloodstream infections.1
Key takeaway
Patients in the ICU—surgical patients and/or those whose treatment includes the use of central lines, catheters or ventilators—are at high risk for HAIs, especially when you consider that their own nose and mouth are major reservoirs for bacteria that can easily shed onto the body. But a universal ICU decolonization protocol that includes daily CHG bathing; nasal decolonization twice a day for up to five days using mupirocin, povidone iodine or ethyl alcohol; and daily oral decolonization can prevent or reduce the risk of harmful HAIs—even the most harmful and pervasive ones like MRSA.
References:
- The Reduce MRSA Trial Working Group, Harvard Pilgrim Healthcare, et al. (2013, September). Universal ICU Decolonization Toolkit: An Enhanced Protocol. Agency for Healthcare Research and Quality. https://www.ahrq.gov/sites/default/files/publications/files/universalicu.pdf
- Quinn, B., and Baker, D. (2015, March). Comprehensive oral care helps prevent hospital-acquired nonventilator pneumonia. American Nurse Today, 10(3), 18-23. https://www.myamericannurse.com/wp-content/uploads/2015/03/ant3-CE-Oral-Care-225.pdf
- Dentistry Today. (2021, January 6). Oral hygiene prevents pneumonia in patients with ventilators. https://www.dentistrytoday.com/oral-hygiene-prevents-pneumonia-in-patients-on-ventilators/